Diagnostic Value of Combined Detection of Serum AIF-1, GDF15, and DCLK1 in Breast Cancer
-
摘要:目的
探讨血清同种异体移植物炎性因子-1(AIF-1)、生长分化因子15(GDF15)、双皮质素样激酶1(DCLK1)联合检测对乳腺癌的诊断价值。
方法选取本院2020年4月至2023年10月期间收治的114例女性乳腺癌患者(乳腺癌组),另选取同期在本院健康体检女性志愿者114例(对照组)。采用酶联免疫吸附法(ELISA)检测血清AIF-1、GDF15、DCLK1水平;多因素Logistic回归分析乳腺癌的危险因素;受试者工作特征(ROC)曲线分析血清AIF-1、GDF15、DCLK1水平对乳腺癌的诊断价值。
结果与对照组相比,乳腺癌组血清AIF-1、GDF15、DCLK1水平均明显升高(P<0.05)。Ⅲ~Ⅳ期、中低分化、有淋巴结转移及Ki-67阳性的乳腺癌患者血清AIF-1、GDF15、DCLK1表达水平显著升高(均P<0.05)。血清AIF-1、GDF15、DCLK1是影响乳腺癌的危险因素,三者单一及联合诊断乳腺癌的曲线下面积(AUC)分别为0.834、0.753、0.861及0.930,联合诊断AUC值显著高于单独评估的AUC值(Z三者联合-AIF-1=3.479、Z三者联合-GDF15=5.147、Z三者联合-DCLK1=3.121,均P<0.05)。
结论乳腺癌患者血清AIF-1、GDF15、DCLK1水平升高,均是影响乳腺癌的危险因素,且三者联合诊断的效能更佳。
-
关键词:
- 乳腺癌 /
- 同种异体移植物炎性因子-1 /
- 生长分化因子15 /
- 双皮质素样激酶1 /
- 诊断
Abstract:ObjectiveTo explore the diagnostic value of the combined detection of serum allograft inflammatory factor-1 (AIF-1), growth differentiation factor-15 (GDF15), and doublecortin-like kinase 1 (DCLK1) in breast cancer.
MethodsA total of 114 female breast cancer patients (breast cancer group) and 114 female volunteers (control group) who underwent physical examination were selected. Enzyme-Linked immunosorbent assay was applied to detect serum levels of AIF-1, GDF15, and DCLK1. Multivariate Logistic regression was used to analyze the risk factors affecting breast cancer. ROC curve was used to analyze the diagnostic value of serum AIF-1, GDF15, DCLK1 levels in breast cancer.
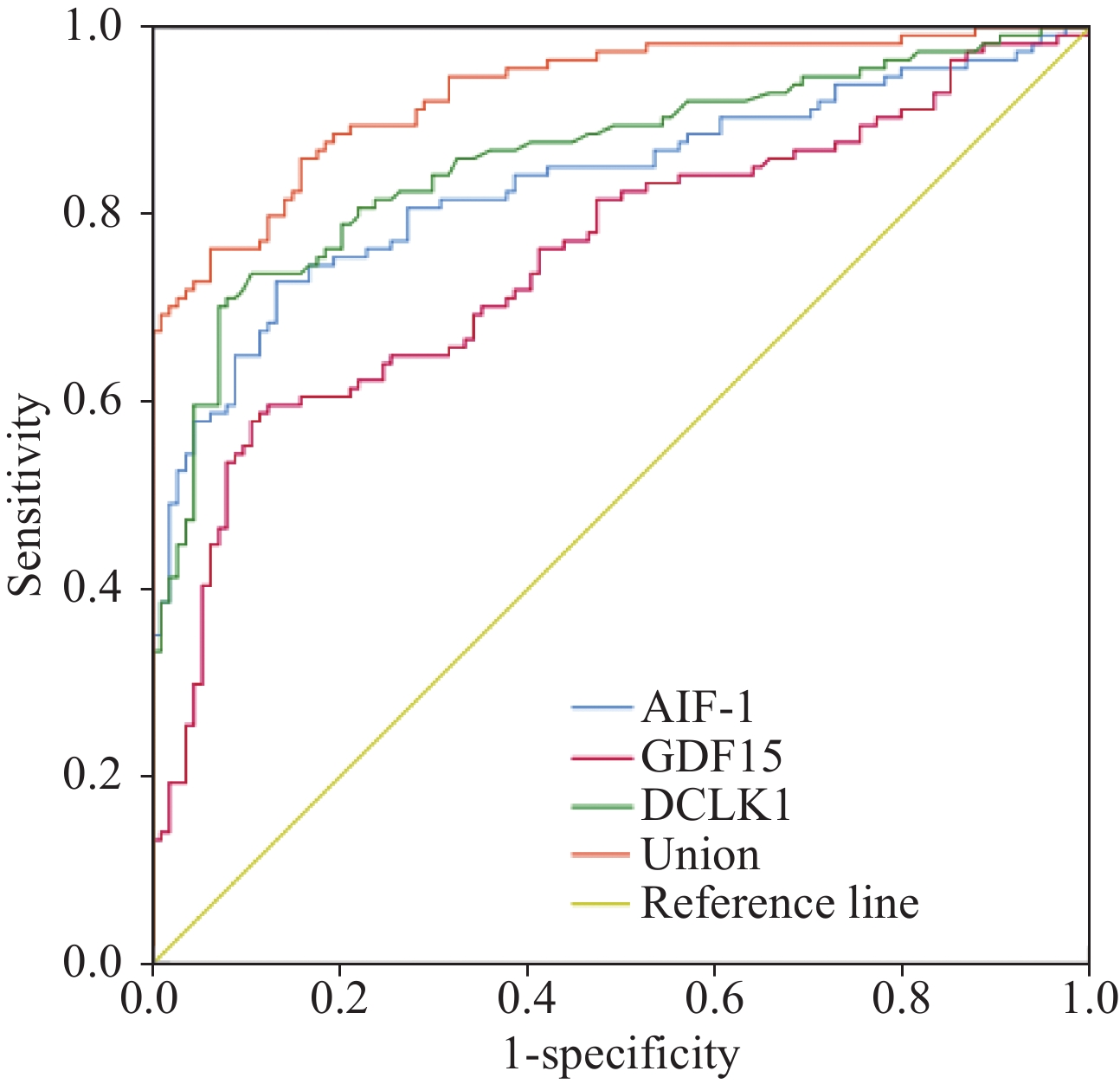
ResultsThe serum levels of AIF-1, GDF15, and DCLK1 in the breast cancer group were obviously higher than those of the control group (P<0.05). The expression levels of serum AIF-1, GDF15, and DCLK1 were significantly elevated in breast cancer patients with stage Ⅲ-Ⅳ, moderate and poor differentiation, lymph-node metastasis, and Ki-67 positive (P<0.05). Serum AIF-1, GDF15, and DCLK1 were risk factors for breast cancer, and the areas under the curve (AUC) for single and combined diagnosis of breast cancer for all three were 0.834, 0.753, 0.861, and 0.930, respectively. Additionally, the combined diagnosis AUC values were significantly higher than those assessed alone (Zcombination-AIF-1=3.479, Zcombination-GDF15=5.147, and Zcombination-DCLK1=3.121; all P<0.05).
ConclusionIn breast cancer patients, the serum AIF-1, GDF15, and DCLK1 levels increase. They are risk factors for breast cancer, and the combined diagnosis of the three is more effective.
-
0 引言
乳腺癌是在多种致癌因素的作用下,乳腺上皮组织增殖失控而形成的一种恶性肿瘤,具有特定的生物学行为和病理学特征,是女性最常见的一种恶性肿瘤[1],其发病机制复杂[2]。目前乳腺癌的筛查以影像学检查为主,乳房X线、超声及MRI是最常用的方式,由于早期肿块形成不明显且边界不清楚,导致诊断具有一定的假阳性[3],因此,寻找与乳腺癌相关的生物学标志物,对其准确诊断具有重要意义。同种异体移植物炎性因子-1(Allograft inflammatory factor-1, AIF-1)是一种由巨噬细胞、单核细胞和中性粒细胞产生的胞质蛋白,可以分泌到细胞外,并可以作为细胞因子发挥作用,其过度表达与肿瘤发生和转移相关[4]。生长分化因子15(Growth differentiation factor-15, GDF15)是转化生长因子β超家族的一个分支成员,在癌症、心脏代谢障碍和其他疾病中发挥多种病理生理作用,在肿瘤微环境中,GDF15由肿瘤相关成纤维细胞和巨噬细胞表达,与低存活率相关,是癌症进展的标志[5]。双皮质素样激酶1(Doublecortin-like kinase 1, DCLK1)是一种蛋白质分子,在各种癌症转移中起着至关重要的作用,与许多干细胞受体、信号通路和基因的表达相关,在促进肿瘤发生中起直接或间接作用[6]。目前关于AIF-1、GDF15、DCLK1在乳腺癌中的研究鲜有报道,基于此,本研究通过检测其在乳腺癌中的表达,并分析其对乳腺癌的诊断价值,以期为临床诊治提供一定的参考依据。
1 资料与方法
1.1 研究对象
选取本院2020年4月至2023年10月期间收治的114例女性乳腺癌患者(乳腺癌组),年龄37~64岁,平均年龄(50.69±5.86)岁,平均体质量指数(Body mass index, BMI)(21.23±1.34)kg/m2;另选取同期在本院健康体检的女性志愿者114例(对照组),年龄33~60(50.82±5.62)岁,平均BMI(21.43±1.52)kg/m2。两组一般资料比较差异无统计学意义(P>0.05),具有可比性。本研究经本院伦理委员会审核批准(批号:2019—12091)。
1.2 纳入与排除标准
纳入标准:(1)乳腺癌患者符合《中国抗癌协会乳腺癌诊治指南与规范(2019年版)》[7]中相关诊断标准并经病理学确诊;(2)首次确诊者;(3)患者及家属知情并签署知情同意书;(4)临床资料完整者。排除标准:(1)合并有其他恶性肿瘤者;(2)合并有免疫系统疾病者;(3)严重心肝肾功能异常者;(4)妊娠期、哺乳期女性;(5)凝血功能障碍者;(6)合并有严重的精神障碍疾病者;(7)发生远处转移者。
1.3 方法
1.3.1 血清及一般资料收集
收集乳腺癌患者确诊后次日及健康体检志愿者体检当日清晨空腹静脉血5 ml,室温下静置30 min,于4℃下1 000 g离心15 min,收集上清液,置于−80℃保存待测。另收集乳腺癌患者年龄、病理类型、临床分期、分化程度、有无淋巴结转移、是否绝经、肿瘤直径、雌激素受体(Estrogen receptor, ER)、人表皮生长因子受体-2(Human epidermal growth factor receptor 2, HER-2)、孕激素受体(Progesterone receptor, PR)、细胞核增殖抗原(Ki-67)等信息。
1.3.2 血清AIF-1、GDF15、DCLK1水平检测
采用酶联免疫吸附法(Enzyme-linked immunosorbnent assay, ELISA)检测所有研究对象血清中AIF-1(上海柯雷生物科技有限公司,货号:E5124)、GDF15(上海莼试生物技术有限公司,货号:CS-2539E)、DCLK1(武汉艾美捷科技有限公司,货号:EKU03792)水平。
1.4 统计学方法
采用统计软件SPSS25.0处理数据,符合正态分布的计量资料以均数±标准差($ \bar x \pm s $)表示,两组间比较行t检验。采用单因素和多因素Logistic回归分析影响乳腺癌的危险因素;采用受试者工作特征(Receiver operating characteristic, ROC)曲线分析血清AIF-1、GDF15、DCLK1水平对乳腺癌的诊断价值,ROC曲线下面积(Area under the curve, AUC)比较采用Z检验。以P<0.05代表差异具有统计学意义。
2 结果
2.1 两组血清AIF-1、GDF15、DCLK1水平比较
与对照组相比,乳腺癌组血清AIF-1、GDF15、DCLK1水平均明显升高(P<0.05),见表1。
表 1 两组血清AIF-1、GDF15、DCLK1水平比较 ($ \bar x \pm s $)Table 1 Comparison of serum AIF-1, GDF15, and DCLK1 levels between two groups ($ \bar x \pm s $)Groups AIF-1(pg/ml) GDF15(pg/ml) DCLK1(ng/ml) Breast cancer 263.45±85.62 560.65±183.48 4.16±1.24 Control 176.57±55.48 375.24±123.51 2.64±0.75 t 9.092 8.950 11.199 P <0.001 <0.001 <0.001 Notes: AIF-1: allograft inflammatory factor-1; GDF15: growth differentiation factor-15;DCLK1: doublecortin-like kinase 1. 2.2 血清AIF-1、GDF15、DCLK1水平与临床病理特征的关系
Ⅲ~Ⅳ期、中低分化、有淋巴结转移及Ki-67阳性的乳腺癌患者血清AIF-1、GDF15、DCLK1表达水平分别高于Ⅰ~Ⅱ期、高分化、无淋巴结转移及Ki-67阴性患者(P<0.05),而不同年龄、病理类型、绝经、肿瘤直径、ER、HER-2及PR水平患者间比较无显著性差异(P>0.05),见表2。
表 2 乳腺癌患者血清AIF-1、GDF15、DCLK1水平与临床病理特征的关系($ \bar x \pm s $)Table 2 Relationship between serum AIF-1, GDF15, DCLK1 levels and clinical pathological characteristics ($ \bar x \pm s $)Clinical features n AIF-1(pg/ml) t P GDF15(pg/ml) t P DCLK1(ng/ml) t P Age (years) ≥50 53 265.06±81.65 561.33±181.21 4.18±1.12 <50 61 262.05±82.34 560.06±182.63 4.14±1.14 Pathological type 0.117 0.907 0.069 0.945 0.225 0.822 Infiltrating ductal carcinoma 98 263.81±81.56 561.12±178.64 4.17±1.16 Other 16 261.24±82.47 557.77±181.02 4.10±1.11 Clinical stages 5.620 <0.001 6.753 0.000 12.343 <0.001 Ⅰ-Ⅱ 68 229.51±75.64 469.57±142.31 3.14±0.87 Ⅲ-Ⅳ 46 313.62±82.34 695.29±214.81 5.67±1.32 Differentiation degree 6.968 <0.001 5.466 0.000 6.762 <0.001 Well 35 201.36±58.64 442.08±124.51 3.10±0.75 Moderate to poor 79 290.96±65.27 613.18±165.43 4.63±1.24 Lymph node metastasis 6.182 <0.001 5.807 0.000 7.363 <0.001 Yes 72 297.79±87.45 630.36±187.62 4.79±1.36 No 42 204.58±56.82 441.15±126.35 3.08±0.87 Menopause 0.278 0.781 0.034 0.973 0.291 0.772 Yes 67 261.69±80.31 560.16±184.36 4.13±1.26 No 47 265.96±81.24 561.35±181.09 4.20±1.27 Tumor diameter (cm) 0.235 0.815 0.195 0.846 1.185 0.239 ≥2 76 264.65±76.48 562.86±169.47 4.25±1.16 <2 38 261.05±78.52 556.23±175.32 3.98±1.12 Ki-67 7.706 <0.001 6.488 0.000 6.107 <0.001 Negative 51 196.15±65.37 451.19±127.54 3.42±1.05 Positive 63 317.93±96.28 649.26±185.28 4.76±1.25 ER 0.142 0.887 0.088 0.930 0.568 0.571 Negative 59 264.54±84.17 562.04±173.48 4.22±1.21 Positive 55 262.28±85.23 559.16±176.24 4.10±1.03 HER-2 0.172 0.863 0.065 0.948 0.338 0.736 Negative 44 265.14±82.43 562.02±179.47 4.21±1.26 Positive 70 262.39±83.17 559.79±176.34 4.13±1.21 PR 0.125 0.901 0.025 0.980 0.278 0.782 Negative 63 264.35±85.24 561.04±183.64 4.19±1.32 Positive 51 262.34±85.18 560.17±182.75 4.12±1.36 Notes: ER: estrogen receptor; HER-2: human epidermal growth factor receptor 2; PR: progesterone receptor. 2.3 多因素Logistic回归分析影响乳腺癌发生的因素
以乳腺癌患病情况(0=否,1=是)作为因变量,将年龄(≥50=1,<50=0)、病理类型(浸润性导管癌=1,其他=0)、临床分期(Ⅲ~Ⅳ期=1,Ⅰ~Ⅱ期=0)、分化程度(中、低分化=1,高分化=0)、淋巴结转移(有=1,无=0)、绝经(否=1,是=0)、肿瘤直径(≥2=1,<2=0)、Ki-67表达(阳性=1,阴性=0)、ER表达(阳性=1,阴性=0)、HER-2表达(阳性=1,阴性=0)、PR表达(阳性=1,阴性=0)以及血清AIF-1(实测值)、GDF15(实测值)、DCLK1水平(实测值)作为自变量,进行单因素Logistic回归分析,结果显示血清AIF-1、GDF15、DCLK1、分化程度、淋巴结转移是影响乳腺癌的因素。进一步将上述差异有统计学意义的指标进行多因素Logistic回归分析,结果显示,血清AIF-1、GDF15、DCLK1是影响乳腺癌的危险因素(P<0.05),见表3~4。
表 3 影响乳腺癌发生的单因素Logistic回归分析Table 3 Univariate Logistic regression analysis of factors affecting the occurrence of breast cancerIndependent variable β SE Waldχ2 P OR 95%CI Age 0.430 0.316 1.850 0.174 1.537 0.827-2.855 Pathological type 0.584 0.364 2.578 0.108 1.794 0.879-3.662 Clinical stages 0.660 0.381 3.002 0.083 1.935 0.917-4.083 Differentiation degree 0.863 0.332 6.762 0.009 2.371 1.237-4.545 Lymph node metastasis 0.938 0.359 6.833 0.009 2.556 1.265-5.166 Menopause 0.200 0.399 0.250 0.617 1.221 0.559-2.669 Tumor diameter 0.506 0.347 2.123 0.145 1.658 0.840-3.273 Ki-67 0.380 0.315 1.454 0.228 1.462 0.789-2.711 ER 0.469 0.294 2.549 0.110 1.599 0.899-2.845 HER-2 0.603 0.346 3.034 0.082 1.827 0.928-3.600 PR 0.533 0.328 2.640 0.104 1.704 0.896-3.241 AIF-1 0.955 0.274 12.151 <0.001 2.599 1.519-4.447 GDF15 1.104 0.291 14.400 <0.001 3.017 1.706-5.337 DCLK1 1.271 0.376 11.430 0.001 3.565 1.706-7.449 表 4 影响乳腺癌发生的多因素Logistic回归分析Table 4 Multivariate Logistic regression analysis of factors affecting the occurrence of breast cancerIndependent variable β SE Waldχ2 P OR 95%CI AIF-1 1.015 0.307 10.920 0.001 2.758 1.511-5.034 GDF15 1.185 0.268 19.554 <0.001 3.271 1.934-5.531 DCLK1 1.269 0.292 18.884 <0.001 3.557 2.007-6.304 Differentiation degree 0.689 0.375 3.377 0.066 1.992 0.955-4.154 Lymph node metastasis 0.623 0.351 3.153 0.076 1.865 0.937-3.711 2.4 血清AIF-1、GDF15、DCLK1水平对乳腺癌的诊断价值
以乳腺癌患病情况(0=否,1=是)作为因变量,以血清AIF-1、GDF15、DCLK1水平(实测值)作为检验变量绘制ROC曲线。血清AIF-1诊断乳腺癌的曲线下面积为0.834(95%CI:0.780~0.880),敏感度和特异性分别为72.81%、86.84%,最佳截断值为218.59 pg/ml;血清GDF15诊断乳腺癌的AUC为0.753(95%CI:0.692~0.808),敏感度和特异性分别为58.77%、88.60%,最佳截断值为511.56 pg/ml;血清DCLK1诊断乳腺癌的AUC为0.861(95%CI:0.809~0.903),敏感度和特异性分别为73.68%、89.47%,最佳截断值为3.51 ng/ml;血清AIF-1、GDF15、DCLK1联合诊断乳腺癌的AUC为0.930(95%CI:0.889~0.960),敏感度和特异性分别为85.96%、84.21%。三者联合诊断乳腺癌的AUC显著高于血清AIF-1、GDF15、DCLK1单独评估(Z三者联合-AIF-1=3.479、Z三者联合-GDF15=5.147、Z三者联合-DCLK1=3.121,均P<0.05),见图1。
3 讨论
乳腺癌是全球范围内发病率和死亡率最高的恶性肿瘤,遗传和临床异质性特征明显,具有独特的体细胞突变并伴随着基因和蛋白质表达的变化,其中调控肿瘤发生和发展分子机制的复杂性决定了其异质性,通常通过侵袭性、形态学、免疫组织化学标记的表达以及基因组来分类[8]。乳房X线是早期诊断的主要方法之一,但具有较高的假阳性,对致密乳腺组织的敏感度较低,通常被检测到时,部分患者已经存在淋巴结转移、扩散,导致不良预后[9]。因此,及时对乳腺癌进行有效诊断,及早采取干预措施对其预后尤为关键。
AIF-1是位于6p21.3上的一种钙结合蛋白,其合成受干扰素-γ的调控,具有细胞信号蛋白的特征,其过表达可促进细胞的增殖、迁移和活化[10]。AIF-1是一类重要的天然免疫分子,能特异性表达于单核/巨噬细胞及嗜中性粒细胞上,通过募集巨噬细胞到病灶部位,发挥免疫调控作用[11]。Wang等[12]研究表明,AIF-1在多种肿瘤中均高度表达,在人非小细胞肺癌组织中显著上调,与患者预后密切相关,且与肿瘤分期和转移正相关。本研究显示乳腺癌组血清AIF-1水平显著升高,与Sikora等[13]研究结果相符,提示AIF-1参与乳腺疾病的发生,推测AIF-1水平升高可能会促进癌细胞增殖和迁移,进而参与乳腺癌的发生。本研究还发现血清AIF-1的表达与临床病理特征密切相关,且血清AIF-1是影响乳腺癌的危险因素,表明AIF-1水平的升高可增加乳腺癌的风险,其具有一定的乳腺癌诊断价值。
GDF15是一种相对分子质量为25 kDa的同型二聚体,属于转化生长因子β超家族成员,是一种血浆中循环的分泌蛋白,又称为巨噬细胞抑制因子-1,位于人类染色体19p13.11上,由N-末端信号肽组成,用于分泌和运输[14]。GDF15是一种在组织损伤、缺氧、炎性细胞因子等刺激下产生的细胞因子,参与细胞与组织内稳态的调控[15]。Ahmed等[16]研究发现GDF15在许多晚期癌症中过度表达,与患者存活率负相关,与肿瘤进展、组织病理学分级相关,可能是肿瘤生物标志物之一。本研究结果显示,乳腺癌组血清GDF15水平显著高于对照组,并且在Ⅲ~Ⅳ期、中低分化、有淋巴结转移及Ki-67阳性患者中显著升高,与Ahmed等[16]研究结果相似,提示血清GDF15水平与乳腺癌的发生发展有关。另有研究表明,在具有较大肿瘤、晚期疾病阶段和远处转移的乳腺癌患者中,血清GDF15水平显著升高,其表达与淋巴结转移呈正相关,可以作为一个独立的早期诊断标志物,并且比CA15-3具有更好的预测能力[17]。Zhao等[18]研究发现GDF15在乳腺癌患者中呈高表达,可作为一种新的标志物和乳腺癌放疗的潜在治疗靶点。多因素Logistic回归分析显示,血清GDF15是影响乳腺癌的危险因素,表明GDF15水平的升高可增加乳腺癌的风险。ROC曲线分析证实了血清GDF15对乳腺癌具有一定诊断价值,与Zhao等[18]研究结果相符,提示GDF15参与乳腺癌的发生发展。
DCLK1是一种蛋白激酶,属于存在于细胞质中的微管相关蛋白双皮质素家族,由两个末端组成,具有微管相关功能,在各种癌症中过度表达[19]。研究表明,DCLK1的表达与神经发生和人类癌症有关,被用作肿瘤细胞标志物[20]。Gzil等[21]研究表明,乳腺癌细胞中的DCLK1具有癌干细胞样特性,随着其水平的增加相关通路被激活,促进了乳腺恶性肿瘤进展,表明DCLK1是乳腺癌的一个潜在早期诊断指标。本研究表明,乳腺癌组血清DCLK1水平显著升高,并且与临床病理特征相关。提示DCLK1参与乳腺癌的发生和发展。进一步多因素Logistic回归分析显示,血清DCLK1是乳腺癌的危险因素,且经ROC曲线分析证实,DCLK1对乳腺癌具有一定的诊断价值,联合AIF-1、DCLK1诊断的效能更佳。
综上所述,乳腺癌患者血清AIF-1、GDF15、DCLK1水平均升高,与临床病例特征相关,均是影响乳腺癌的危险因素,三者联合具有较高的诊断效能。但本研究尚有不足之处,上述内容提及AIF-1在人非小细胞肺癌组织中也异常表达,其诊断乳腺癌可能缺乏组织特异性,且本研究尚未分析AIF-1、GDF15、DCLK1在乳腺癌中的具体作用机制及预后价值,后续研究也将进一步明确AIF-1对乳腺癌的诊断价值,并对本研究结果加以验证。
Competing interests: The authors declare that they have no competing interests.利益冲突声明:所有作者均声明不存在利益冲突。作者贡献:夏利敏:研究设计和实施、数据分析、查阅文献、撰写文章霍永平:研究设计、查阅文献马祥敏:数据分析、统计分析陈世豪:文章审阅 -
表 1 两组血清AIF-1、GDF15、DCLK1水平比较 ($ \bar x \pm s $)
Table 1 Comparison of serum AIF-1, GDF15, and DCLK1 levels between two groups ($ \bar x \pm s $)
Groups AIF-1(pg/ml) GDF15(pg/ml) DCLK1(ng/ml) Breast cancer 263.45±85.62 560.65±183.48 4.16±1.24 Control 176.57±55.48 375.24±123.51 2.64±0.75 t 9.092 8.950 11.199 P <0.001 <0.001 <0.001 Notes: AIF-1: allograft inflammatory factor-1; GDF15: growth differentiation factor-15;DCLK1: doublecortin-like kinase 1. 表 2 乳腺癌患者血清AIF-1、GDF15、DCLK1水平与临床病理特征的关系($ \bar x \pm s $)
Table 2 Relationship between serum AIF-1, GDF15, DCLK1 levels and clinical pathological characteristics ($ \bar x \pm s $)
Clinical features n AIF-1(pg/ml) t P GDF15(pg/ml) t P DCLK1(ng/ml) t P Age (years) ≥50 53 265.06±81.65 561.33±181.21 4.18±1.12 <50 61 262.05±82.34 560.06±182.63 4.14±1.14 Pathological type 0.117 0.907 0.069 0.945 0.225 0.822 Infiltrating ductal carcinoma 98 263.81±81.56 561.12±178.64 4.17±1.16 Other 16 261.24±82.47 557.77±181.02 4.10±1.11 Clinical stages 5.620 <0.001 6.753 0.000 12.343 <0.001 Ⅰ-Ⅱ 68 229.51±75.64 469.57±142.31 3.14±0.87 Ⅲ-Ⅳ 46 313.62±82.34 695.29±214.81 5.67±1.32 Differentiation degree 6.968 <0.001 5.466 0.000 6.762 <0.001 Well 35 201.36±58.64 442.08±124.51 3.10±0.75 Moderate to poor 79 290.96±65.27 613.18±165.43 4.63±1.24 Lymph node metastasis 6.182 <0.001 5.807 0.000 7.363 <0.001 Yes 72 297.79±87.45 630.36±187.62 4.79±1.36 No 42 204.58±56.82 441.15±126.35 3.08±0.87 Menopause 0.278 0.781 0.034 0.973 0.291 0.772 Yes 67 261.69±80.31 560.16±184.36 4.13±1.26 No 47 265.96±81.24 561.35±181.09 4.20±1.27 Tumor diameter (cm) 0.235 0.815 0.195 0.846 1.185 0.239 ≥2 76 264.65±76.48 562.86±169.47 4.25±1.16 <2 38 261.05±78.52 556.23±175.32 3.98±1.12 Ki-67 7.706 <0.001 6.488 0.000 6.107 <0.001 Negative 51 196.15±65.37 451.19±127.54 3.42±1.05 Positive 63 317.93±96.28 649.26±185.28 4.76±1.25 ER 0.142 0.887 0.088 0.930 0.568 0.571 Negative 59 264.54±84.17 562.04±173.48 4.22±1.21 Positive 55 262.28±85.23 559.16±176.24 4.10±1.03 HER-2 0.172 0.863 0.065 0.948 0.338 0.736 Negative 44 265.14±82.43 562.02±179.47 4.21±1.26 Positive 70 262.39±83.17 559.79±176.34 4.13±1.21 PR 0.125 0.901 0.025 0.980 0.278 0.782 Negative 63 264.35±85.24 561.04±183.64 4.19±1.32 Positive 51 262.34±85.18 560.17±182.75 4.12±1.36 Notes: ER: estrogen receptor; HER-2: human epidermal growth factor receptor 2; PR: progesterone receptor. 表 3 影响乳腺癌发生的单因素Logistic回归分析
Table 3 Univariate Logistic regression analysis of factors affecting the occurrence of breast cancer
Independent variable β SE Waldχ2 P OR 95%CI Age 0.430 0.316 1.850 0.174 1.537 0.827-2.855 Pathological type 0.584 0.364 2.578 0.108 1.794 0.879-3.662 Clinical stages 0.660 0.381 3.002 0.083 1.935 0.917-4.083 Differentiation degree 0.863 0.332 6.762 0.009 2.371 1.237-4.545 Lymph node metastasis 0.938 0.359 6.833 0.009 2.556 1.265-5.166 Menopause 0.200 0.399 0.250 0.617 1.221 0.559-2.669 Tumor diameter 0.506 0.347 2.123 0.145 1.658 0.840-3.273 Ki-67 0.380 0.315 1.454 0.228 1.462 0.789-2.711 ER 0.469 0.294 2.549 0.110 1.599 0.899-2.845 HER-2 0.603 0.346 3.034 0.082 1.827 0.928-3.600 PR 0.533 0.328 2.640 0.104 1.704 0.896-3.241 AIF-1 0.955 0.274 12.151 <0.001 2.599 1.519-4.447 GDF15 1.104 0.291 14.400 <0.001 3.017 1.706-5.337 DCLK1 1.271 0.376 11.430 0.001 3.565 1.706-7.449 表 4 影响乳腺癌发生的多因素Logistic回归分析
Table 4 Multivariate Logistic regression analysis of factors affecting the occurrence of breast cancer
Independent variable β SE Waldχ2 P OR 95%CI AIF-1 1.015 0.307 10.920 0.001 2.758 1.511-5.034 GDF15 1.185 0.268 19.554 <0.001 3.271 1.934-5.531 DCLK1 1.269 0.292 18.884 <0.001 3.557 2.007-6.304 Differentiation degree 0.689 0.375 3.377 0.066 1.992 0.955-4.154 Lymph node metastasis 0.623 0.351 3.153 0.076 1.865 0.937-3.711 -
[1] Zannetti A. Breast Cancer: From Pathophysiology to Novel Therapeutic Approaches 2.0[J]. Int J Mol Sci, 2023, 24(3): 2542-2553. doi: 10.3390/ijms24032542
[2] Ben-Dror J, Shalamov M, Sonnenblick A. The History of Early Breast Cancer Treatment[J]. Genes (Basel), 2022, 13(6): 960-964. doi: 10.3390/genes13060960
[3] Lee Y, Ni J, Beretov J, et al. Recent advances of small extracellular vesicle biomarkers in breast cancer diagnosis and prognosis[J]. Mol Cancer, 2023, 22(1): 33-39. doi: 10.1186/s12943-023-01741-x
[4] Guijarro LG, Cano-Martínez D, Toledo-Lobo MV, et al. Evaluation of AIF-1 (Allograft Inflammatory Factor-1) as a Biomarker of Crohn's Disease Severity[J]. Biomedicines, 2022, 10(3): 727-735. doi: 10.3390/biomedicines10030727
[5] Siddiqui JA, Pothuraju R, Khan P, et al. Pathophysiological role of growth differentiation factor 15 (GDF15) in obesity, cancer, and cachexia[J]. Cytokine Growth Factor Rev, 2022, 64(1): 71-83.
[6] Chhetri D, Vengadassalapathy S, Venkadassalapathy S, et al. Pleiotropic effects of DCLK1 in cancer and cancer stem cells[J]. Front Mol Biosci, 2022, 9: 965730-965738. doi: 10.3389/fmolb.2022.965730
[7] 中国抗癌协会乳腺癌专业委员会. 中国抗癌协会乳腺癌诊治指南与规范(2019年版)[J]. 中国癌症杂志, 2019, 29(8): 609-680. [The Society of Breast Cancer of China Anti-CancerAssociation. Chinese Cancer Association Guidelines for Breast Cancer Diagnosis and Treatment(2019 Edition)[J]. Zhongguo Ai Zeng Za Zhi, 2019, 29(8): 609-680.] The Society of Breast Cancer of China Anti-CancerAssociation. Chinese Cancer Association Guidelines for Breast Cancer Diagnosis and Treatment(2019 Edition)[J]. Zhongguo Ai Zeng Za Zhi, 2019, 29(8): 609-680.
[8] 姜斌, 徐浩, 张宇聪, 等. 血清前列腺特异性抗原在乳腺癌中表达水平的变化及诊断价值的Meta分析[J]. 中华实验外科杂志, 2020, 37(7): 1212-1214. [Jiang B, Xu Hao, Zhang YC, et al. A Meta analysis of expression level change and diagnosis value of serum prostate specificantigen in patients with breast cancer[J]. Zhonghua Shi Yan Wai Ke Za Zhi, 2020, 37(7): 1212-1214.] doi: 10.3760/cma.j.cn421213-20200709-00498 Jiang B, Xu Hao, Zhang YC, et al. A Meta analysis of expression level change and diagnosis value of serum prostate specificantigen in patients with breast cancer[J]. Zhonghua Shi Yan Wai Ke Za Zhi, 2020, 37(7): 1212-1214. doi: 10.3760/cma.j.cn421213-20200709-00498
[9] Houghton SC, Hankinson SE. Cancer Progress and Priorities: Breast Cancer[J]. Cancer Epidemiol Biomarkers Prev, 2021, 30(5): 822-844. doi: 10.1158/1055-9965.EPI-20-1193
[10] Piotrowska K, Słuczanowska-Głabowska S, Kurzawski M, et al. Over-Expression of Allograft Inflammatory Factor-1 (AIF-1) in Patients with Rheumatoid Arthritis[J]. Biomolecules, 2020, 10(7): 1064-1071. doi: 10.3390/biom10071064
[11] Vizioli J, Verri T, Pagliara P. Allograft Inflammatory Factor-1 in Metazoans: Focus on Invertebrates[J]. Biology (Basel), 2020, 9(11): 355-361.
[12] Wang L, Zhao X, Zheng H, et al. AIF-1, a potential biomarker of aggressive tumor behavior in patients with non-small cell lung cancer[J]. PLoS One, 2022, 17(12): e0279211. doi: 10.1371/journal.pone.0279211
[13] Sikora M, Kopeć B, Piotrowska K, et al. Role of allograft inflammatory factor-1 in pathogenesis of diseases[J]. Immunol Lett, 2020, 218: 1-4. doi: 10.1016/j.imlet.2019.12.002
[14] Ma Y, Du J, Chen M, et al. Mitochondrial DNA methylation is a predictor of immunotherapy response and prognosis in breast cancer: scRNA-seq and bulk-seq data insights[J]. Front Immunol, 2023, 14: 1219652. doi: 10.3389/fimmu.2023.1219652
[15] Baek SJ, Eling T. Growth differentiation factor 15 (GDF15): A survival protein with therapeutic potential in metabolic diseases[J]. Pharmacol Ther, 2019, 198: 46-58. doi: 10.1016/j.pharmthera.2019.02.008
[16] Ahmed DS, Isnard S, Lin J, et al. GDF15/GFRAL Pathway as a Metabolic Signature for Cachexia in Patients with Cancer[J]. J Cancer, 2021, 12(4): 1125-1132. doi: 10.7150/jca.50376
[17] Huang JY, Wang YY, Lo S, et al. Visfatin Mediates Malignant Behaviors through Adipose-Derived Stem Cells Intermediary in Breast Cancer[J]. Cancers (Basel), 2019, 12(1): 29-35. doi: 10.3390/cancers12010029
[18] Zhao X, Liu X, Hu S, et al. GDF15 Contributes to Radioresistance by Mediating the EMT and Stemness of Breast Cancer Cells[J]. Int J Mol Sci, 2022, 23(18): 10911-10918. doi: 10.3390/ijms231810911
[19] Huang Z, Shen S, Han X, et al. Macrophage DCLK1 promotes atherosclerosis via binding to IKKβ and inducing inflammatory responses[J]. EMBO Mol Med, 2023, 15(5): 17198-17203. doi: 10.15252/emmm.202217198
[20] Venkat A, Watterson G, Byrne DP, et al. Mechanistic and evolutionary insights into isoform-specific 'supercharging' in DCLK family kinases[J]. Elife, 2023, 12: RP87958. doi: 10.7554/eLife.87958
[21] Gzil A, Szylberg Ł, Jaworski D, et al. The Essential Role of DCLK1 in Pathogenesis, Diagnostic Procedures and Prognostic Stratification of Colorectal Cancer[J]. Anticancer Res, 2019, 39(6): 2689-2697. doi: 10.21873/anticanres.13394



 下载:
下载: