Screening and Identification of Key Genes for Clinical Benefit of Immunotherapy on Lung Adenocarcinoma Based on TCGA Database
-
摘要:目的
基于全基因组测序分析,探索影响肺腺癌免疫疗效预测的关键基因及其可能的机制。
方法选取癌症基因组图谱中肺腺癌数据集(MSKCC, Science 2015)为研究对象,根据免疫治疗疗效持续时间分为两组:持久临床获益组(durable clinical benefit, DCB)和非持久临床获益组(non-durable clinical benefit, Non-DCB)。分析两组之间基因突变谱的差异,进而探索影响肺腺癌免疫治疗的关键分子及潜在生物学功能。
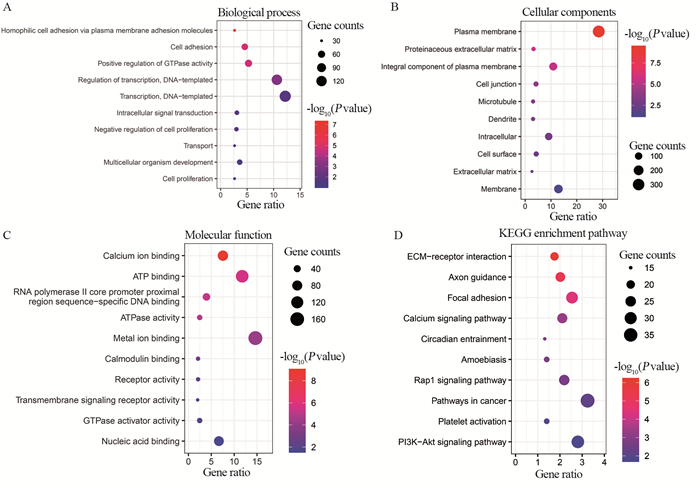
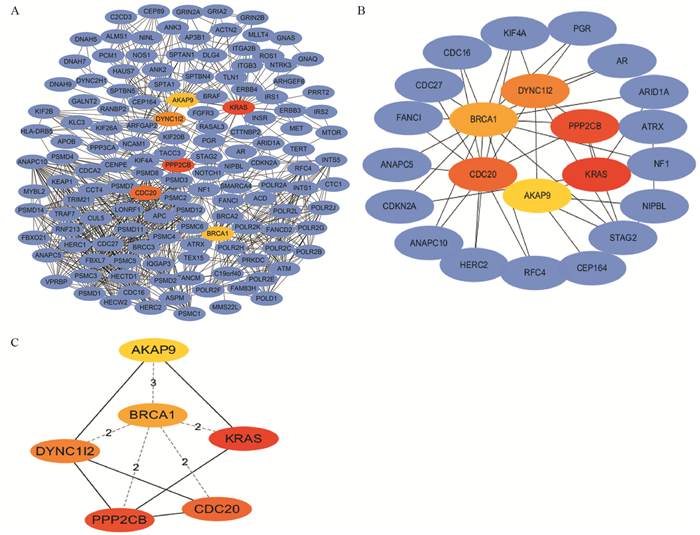
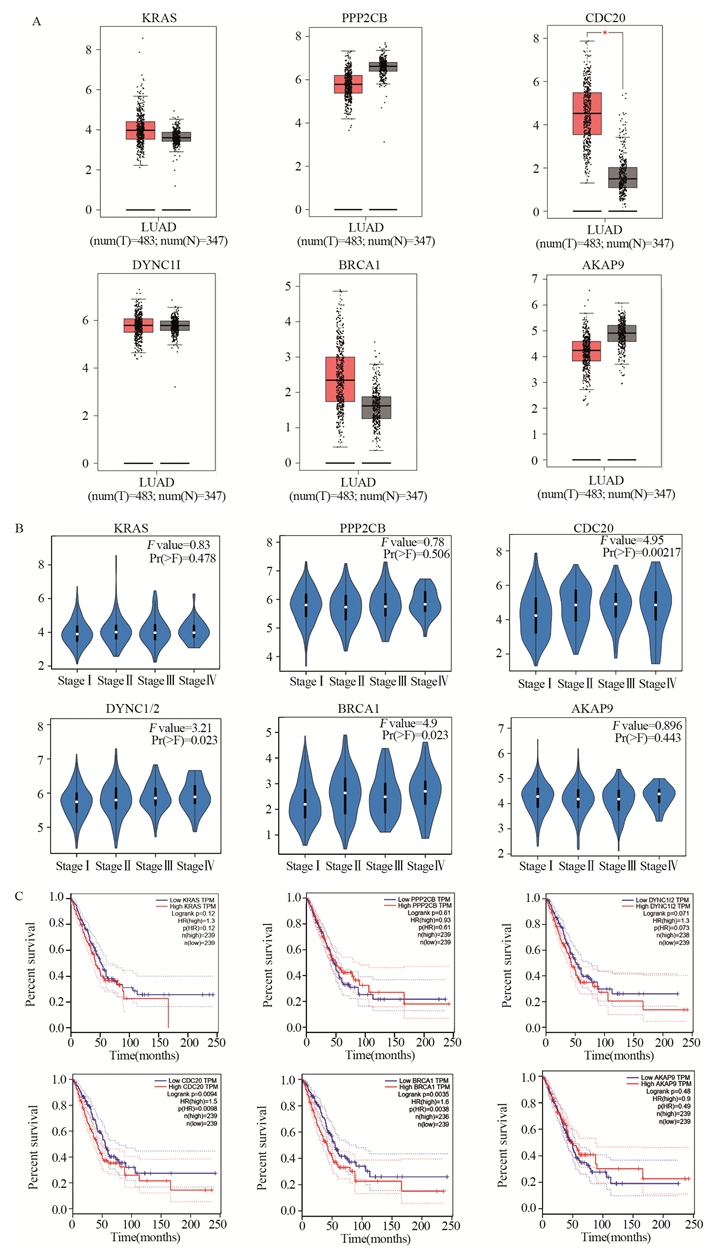
结果基因突变谱在DCB组和Non-DCB组之间存在差异;进一步对DCB组基因突变谱研究,这些基因主要参与了Ca2+通道、Rap1、PI3K-Akt等相关信号通路;蛋白互作网络分析中,筛选出6个节点度最高的核心基因KRAS、PPP2CB、CDC20、DYNCLI2、BRCA1、AKAP9,其中CDC20、BRCA1等基因与肺腺癌患者预后相关。
结论DCB组涉及的关键核心基因有可能指导肺腺癌的免疫特征分型,对于更加精准的免疫治疗具有重要意义。CDC20和BRCA1有可能成为肺腺癌免疫治疗中潜在的治疗靶点。
Abstract:ObjectiveTo identify key biomarkers for predicting the response to immunotherapy and elucidate the possible underlying mechanism in lung adenocarcinoma based on whole-genome sequencing.
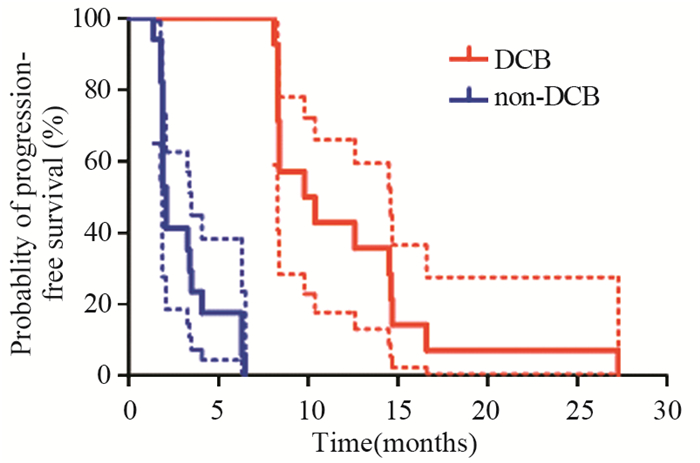
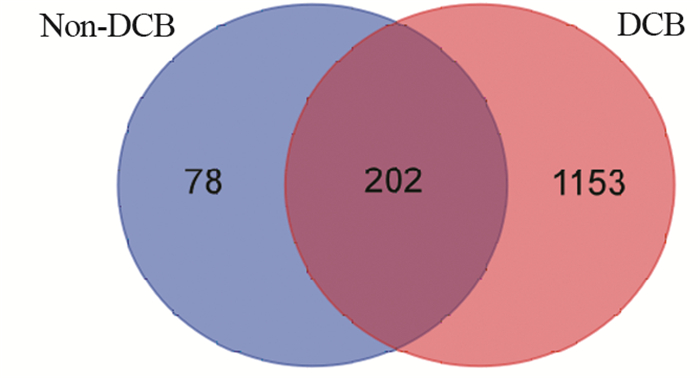
MethodsData set of MSKCC (Science 2015) with lung adenocarcinoma from TCGA database were downloaded. According to the duration time of response to immunotherapy, two groups were divided: durable clinical benefit (DCB) group and non-durable clinical benefit (Non-DCB) group. The differences in gene mutation spectrum between the two groups were analyzed. The key genes and underlying biological functions of immunotherapy for lung adenocarcinoma were further analyzed.
ResultsThere were differences in gene mutation spectrum between the DCB group and the Non-DCB group. In the DCB group, these key genes were mainly involved in Ca signaling pathway, Rap1 and PI3K-AKT pathways. The top 6 hub genes (KRAS, PPP2CB, CDC20, DYNC1I2, BRCA1 and AKAP9) were screened using the PPI network analysis. CDC20 and BRCA1 were associated with the prognosis of lung adenocarcinoma patients.
ConclusionThe hub genes involved in the DCB group might be important to guide the classification of immune signature and improve precision immunotherapy for lung adenocarcinoma. In addition, CDC20 and BRCA1 might be potential therapeutic targets for immunotherapy of lung adenocarcinoma.
-
Key words:
- Lung cancer /
- Immunotherapy /
- Biomarkers /
- TCGA /
- Bioinformatics analysis
-
0 引言
子宫内膜癌是在北美和欧洲最常见的女性恶性肿瘤,近年来我国的发病率明显增加,发病人群年轻化[1]。子宫内膜癌的发病机制目前尚未完全明确,随着研究的深入,越来越清晰地认识到子宫内膜癌是多种因素协同交叉作用、具有不同遗传和分子特征的一类疾病[2-3]。根据肿瘤发病机制与雌激素依赖相关性,将其分为Ⅰ型和Ⅱ型,80%以上为Ⅰ型子宫内膜癌。遗传易感性是导致个体对相同致癌因素敏感度不一致的重要因素,某些雌激素代谢通路中关键酶可以改变体内雌激素或外源性雌激素及其代谢产物的水平。基因多态性与酶活性有关,雌激素代谢酶基因多态性可能导致子宫内膜癌发病易感性差异[4]。本研究利用SNP分型检测技术,探索雌激素代谢关键酶CYP1B1、CYP1A1和NQO1基因的单核苷酸多态性(single nucleotide polymorphisms, SNPs)位点分布频率与Ⅰ型子宫内膜癌易感性之间关系,以期对Ⅰ型子宫内膜癌的易感人群进行筛查。
1 资料与方法
1.1 临床资料
抽取我院2014年3月—2016年10月收治的经病理诊断为子宫内膜样腺癌的103例患者和同期子宫内膜正常的100例其他疾病患者静脉外周全血2~3 ml,作为检测标本。病例和对照组均取得患者的知情同意并详细询问病史,包括初潮年龄、生育状况、绝经年龄、孕产次数、内科并发症及肿瘤家族史。测量身高与体重,并计算体质指数(body mass index, BMI),测量血压,采集静脉血化验空腹血糖(FPG)及血脂、肿瘤标志物[5-6]。年龄31~78岁,平均(51.15±9.69)岁,子宫内膜癌组平均年龄(54.77±8.21)岁,对照组为(46.95±9.65)岁。
1.2 方法
1.2.1 确定候选基因及其SNPs位点
由于Ⅰ型子宫内膜癌为雌激素依赖性肿瘤,结合相关文献报道,在美国国家生物技术信息中心(National Center for Biotechnology Information, NCBI)人类基因组数据库中选择与雌激素代谢相关的关键酶CYP1A1、CYP1B1,具有抗癌突变的依赖还原型辅酶Ⅰ/Ⅱ醌氧化还原酶1(quinone oxido-reductase1, NQO1)3个基因,选取与代谢酶活性密切相关且杂合度大于10%的SNPs位点进行基因型分析。
1.2.2 引物设计合成
利用引物设计软件premier 5.0,在含SNPs的DNA序列上设计PCR引物,并将设计的引物进行引物的同源性比较,选出同源性最小而Tm值和G/C比值合适的引物作为PCR反应引物,所扩增片段应包含要检测的SNPs位点,其位置尽可能设计在PCR扩增片段的中部。
1.2.3 检测方法
使用DNA提取试剂盒(DP304-03)从外周血中提取DNA,进行预扩增,琼脂糖凝胶电泳检测DNA完整性。根据设计引物模板,进行延伸反应及延伸产物纯化。PCR扩增反应体系总体积为50 μl,内含5 μl 10×PCR缓冲液,3 μl 25 mmol/L MgCl2溶液,5 μl 2 mmol/L dNTP混合物,1.25 U Taq DNA聚合酶,0.5 μmol/L引物及100g的基因组DNA。反应在MJ公司PTC-100 PCR反应仪中进行。PCR循环条件为95℃预变性10 min,然后94℃变性30 s,60℃复性30 s,72℃延伸30 s,反应40个循环后,72℃再延伸10 min。扩增产物用2%的琼脂糖凝胶电泳检测,4℃保存。PCR产物经纯化后作为测序模板,用Big-Dye末端荧光标记试剂盒进行测序反应,测序反应产物经纯化后在ABI公司3730XL测序仪上进行测序电泳,用Gene codes公司的Sequencer4.2对测序结果进行分析。
1.3 统计学方法
采用SPSS18.0软件对实验数据进行统计学分析,用χ2检验和多因素Logistic回归模型分析各基因型在两组人群中的分布差异及其与子宫内膜癌临床病理特征的相关性,P < 0.05为差异有统计学意义。
2 结果
2.1 多因素回归分析
CYP1B1基因SNPs位点rs111888224因无碱基改变未纳入统计,rs1056836、rs2551188、rs10916在研究人群中均存在多态性,但分布频率差异无统计学意义;rs1056836 C、G基因分布频率差异有统计学意义(P=0.0454)。
CYP1A1基因SNP位点rs4646421在研究人群中存在CT、CC、TT多态性。与CT型相比,CC型为保护基因型,OR=0.479(95%CI: 0.255~0.899),差异有统计学意义(P=0.0219),其C、T基因分布频率差异有统计学意义(P=0.0041),见表 1。
表 1 基因型/等位基因在Ⅰ型子宫内膜癌患者中的分布(n(%))Table 1 Genotype/alleles distributions in typeⅠendometrial carcinoma cases (n(%))
2.2 CYP1A1基因rs4646421位点多态性与Ⅰ型子宫内膜癌危险因素的分层分析
对CYP1A1基因rs4646421位点不同基因型与Ⅰ型子宫内膜癌的危险因素相关性进行分层比较,发现在年龄 > 60岁、BMI≥25、绝经延迟、并发高血压的个体中,携带CT+TT突变基因型将增加罹患Ⅰ型子宫内膜癌的风险(P < 0.05),见表 2。
表 2 发病危险因素与基因型分布的关系(n(%))Table 2 Association between risk factors and genotypes distributions of SNP(rs4646421) in CYP1A1 (n(%))
3 讨论
雌激素分布在细胞内外表面,通过雌激素受体的核内结合蛋白在靶细胞中保持高亲和力和特异性。涉及雌激素生物合成和代谢的基因的多态性是雌激素受体阳性恶性肿瘤的潜在危险因素,有几种细胞色素P450(CYP)酶参与雌激素的氧化代谢途径[7]。CYP1A1和CYP1B1是代谢产生2-羟基-4-羟基雌激素代谢物的基本酶[8-9],在不同人群中不仅存在多态性,并且在性激素相关组织中的表达高于细胞色素P450超家族的其他成员,其基因多态性与乳腺癌、子宫肌瘤、子宫内膜异位症、宫颈癌等疾病风险相关[10-14]。
CYP1A1基因定位于人类染色体15q22-24,编码由512个氨基酸组成的蛋白质,是细胞色素P450家族中高诱导成员。CYP1A1酶的激活参与内源性和外源性化合物的氧化作用,催化多环芳香族碳氢化合物转化为酚与环氧化合物。一些酚类和环氧化合物可与DNA结合形成加合物,最终转化为致癌物、二醇环氧化物,通过环氧化物水解酶与一些抗肿瘤药物发生耐药,并增加个体肿瘤风险[9, 15]。本研究结果显示CYP1A1基因SNP位点rs4646421在子宫内膜癌人群中存在CT、CC、TT多态性,与携带CT基因型相比,携带CC基因型的个体罹患子宫内膜癌的风险较小,携带T等位基因的个体子宫内膜癌的发病风险高于C等位基因携带者。与携带CC基因型相比,携带TC+TT基因型在年龄 > 60岁、BMI≥25、绝经延迟(超过52岁)、合并高血压的女性中Ⅰ型子宫内膜癌的发病风险增加。
CYP1B1基因位于染色体2q21-22,其单核苷酸多态性SNP总数有353个,目前研究较多的是SNPrs1056836,其mRNA发生1294位碱基胞嘧啶(cytosine, C)变异为鸟嘌呤(guanine, G),使DNA两条链形成野生CC型,杂合CG型和变异GG型3种基因型,即基因多态性。这种改变导致第三外显子432密码子的碱基由CTG变异为GTG,由其编码的亮氨酸(leucine, Leu)变异为缬氨酸(valine, Val),导致CYP1B1酶蛋白功能的改变[16]。CYP1B1通过多方面影响肿瘤的易感性和预后,在胰岛素抵抗中产生作用,突变型表达的酶之蛋白质表现出更强的激活癌前物质活性,或影响睾酮的6β-羟化作用及性激素的激活代谢等[17-18]。
本研究中CYP1B1基因SNP rs2551188、rs10916两个位点在人群中存在多态性,但分布频率无统计学差异;rs1056836在正常子宫内膜组与子宫内膜癌两组间的基因型分布频率无差异,但发生更多的碱基胞嘧啶变异为鸟嘌呤,可能会使罹患子宫内膜癌的风险增加,以往文献中发现对于单个位点基因突变的表现为阴性结论时,多个位点联合的单倍体基因型研究却往往能得到阳性结论,似乎预示着CYP1B1基因在分子遗传学上有一定的倾向性[16-19],但其与肿瘤易感性及预后的机制问题还存在着诸多争议与疑惑,有待于进一步研究。
NQO1是一种重要的化学致癌物质代谢酶,具有抗癌作用,可使内源性及外源性醌类化合物通过电子还原反应变成低毒性的氢醌类物质,再转化为水溶性化合物排出体外,降低了细胞发生突变及癌变的概率。如果位点发生突变,使原位编码的氨基酸发生改变,将会导致该酶活性减弱或完全丧失,降低解毒功能且不能维护细胞稳定,增加某些易感个体细胞发生癌变[20]。报道显示NQO1蛋白高表达在卵巢癌、乳腺癌、结直肠癌等肿瘤中,与临床分期晚、分化程度差和淋巴结转移等临床特征有关[21-22],本研究选择的SNP位点rs45488899和rs1800566虽在两组间均存在基因多态性,但分布频率不具有差异性,因此认为这两个SNP位点与Ⅰ型子宫内膜癌的发生无显著相关性。
本研究通过基因表达谱差异的分析,推测CYP1A1基因rs4646421位点的多态性在Ⅰ型子宫内膜癌的发生发展中起着重要作用,可作为进行高危人群筛查的基因位点,还可以突变的基因型为基础,采取针对性的基因靶向治疗,或者通过修正基因突变谱来改善其预后。但是,基因多态性受复杂的遗传、环境因素、种族等的影响,并与样本量的大小有关,必须经过大样本试验来进一步明确基因多态性与子宫内膜癌易感性之间的基因环境交互作用及具体机制。
Competing interests: The authors declare that they have no competing interests.作者贡献齐晓光:设计实验、分析数据、撰写论文祁春艳、秦博宇:数据分析整理胡毅、韩为东:指导实验,审阅论文 -
表 1 31例晚期持久临床获益与非持久临床获益肺腺癌患者基线特征分析
Table 1 Characteristics of 31 advanced lung adenocarcinoma patients between DCB group and Non-DCB group

表 2 基于Closeness算法评分最高的6个核心关键基因
Table 2 Top 6 hub genes ranked by Closeness method

-
[1] Suresh K, Naidoo J, Lin CT, et al. Immune Checkpoint Immunotherapy for Non-Small Cell Lung Cancer: Benefits and Pulmonary Toxicities[J]. Chest, 2018, 154(6): 1416-1423. doi: 10.1016/j.chest.2018.08.1048
[2] Haanen JB, Robert C. Immune Checkpoint Inhibitors[J]. Prog Tumor Res, 2015, 42: 55-66. http://esmoopen.bmj.com/lookup/external-ref?access_num=25823918&link_type=MED&atom=%2Fesmoopen%2F2%2F4%2Fe000247.atom
[3] Khan M, Lin J, Liao G, et al. Comparative analysis of immune checkpoint inhibitors and chemotherapy in the treatment of advanced non-small cell lung cancer: A meta-analysis of randomized controlled trials[J]. Medicine (Baltimore), 2018, 97(33): e11936. doi: 10.1097/MD.0000000000011936
[4] Janakiram M, Pareek V, Cheng H, et al. Immune checkpoint blockade in human cancer therapy: lung cancer and hematologic malignancies[J]. Immunotherapy, 2016, 8(7): 809-819. doi: 10.2217/imt-2016-0001
[5] Lantuejoul S, Damotte D, Hofman V, et al. Programmed death ligand 1 immunohistochemistry in non-small cell lung carcinoma[J]. J Thorac Dis, 2019, 11(Suppl 1):S89-S101.
[6] Jang HJ, Lee HS, Ramos D, et al. Transcriptome-based molecular subtyping of non-small cell lung cancer may predict response to immune checkpoint inhibitors[J]. J Thorac Cardiovasc Surg, 2019, 159(4): 1589-1610. http://www.researchgate.net/publication/337174405_Transcriptome-based_Molecular_Subtyping_of_Non-Small_Cell_Lung_Cancer_may_Predict_Response_to_Immune_Checkpoint_Inhibitors
[7] Rizvi H, Sanchez-Vega F, La K, et al. Molecular Determinants of Response to Anti-Programmed Cell Death (PD)-1 and Anti-Programmed Death-Ligand 1 (PD-L1) Blockade in Patients With Non-Small-Cell Lung Cancer Profiled With Targeted Next-Generation Sequencing[J]. J Clin Oncol, 2018, 36(7): 633-641.. doi: 10.1200/JCO.2017.75.3384
[8] Gandara DR, Paul SM, Kowanetz M, et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab[J]. Nat Med, 2018, 24(9):1441-1448. doi: 10.1038/s41591-018-0134-3
[9] Wang S, Chen B, Zhu Z, et al. CDC20 overexpression leads to poor prognosis in solid tumors: A system review and meta-analysis[J]. Medicine (Baltimore), 2018, 97(52): e13832. doi: 10.1097/MD.0000000000013832
[10] Alfarsi LH, Ansari RE, Craze ML, et al. CDC20 expression in oestrogen receptor positive breast cancer predicts poor prognosis and lack of response to endocrine therapy[J]. Breast Cancer Res Treat, 2019, 178(3): 535-544. doi: 10.1007/s10549-019-05420-8
[11] Zhang Q, Huang H, Liu A, et al. Cell division cycle 20 (CDC20) drives prostate cancer progression via stabilization of β-catenin in cancer stem-like cells[J]. EBio Medicine, 2019, 42: 397-407. http://www.ncbi.nlm.nih.gov/pubmed/30904606
[12] Cheng S, Castillo V, Sliva D, et al. CDC20 associated with cancer metastasis and novel mushroom-derived CDC20 inhibitors with antimetastatic activity[J]. Int J Oncol, 2019, 54(6): 2250-2256. http://www.researchgate.net/publication/332512404_CDC20_associated_with_cancer_metastasis_and_novel_mushroom-derived_CDC20_inhibitors_with_antimetastatic_activity
[13] Zhang MY, Liu XX, Li H, et al. Elevated mRNA Levels of AURKA, CDC20 and TPX2 are associated with poor prognosis of smoking related lung adenocarcinoma using bioinformatics analysis[J]. Int J Med Sci, 2018, 15(14): 1676-1685. doi: 10.7150/ijms.28728
[14] Yi J, Wei X, Li X, et al. A Genome-Wide Comprehensive Analysis of Alterations in Driver Genes in Non-Small-Cell Lung Cancer[J]. Anticancer Drugs, 2018, 29(1): 10-18. doi: 10.1097/CAD.0000000000000571
[15] Zhang Y, Wang H, Wang J, et al. Global Analysis of Chromosome 1 Genes Among Patients With Lung Adenocarcinoma, Squamous Carcinoma, Large-Cell Carcinoma, Small-Cell Carcinoma, or Non-Cancer[J]. Cancer Metastasis Rev, 2015, 34(2): 249-264. doi: 10.1007/s10555-015-9558-0
[16] Jan Budczies, Carsten Denkert, Balázs Győrffy, et al. Chromosome 9p Copy Number Gains Involving PD-L1 Are Associated With a Specific Proliferation and Immune-Modulating Gene Expression Program Active Across Major Cancer Types[J]. BMC Med Genomics, 2017, 10(1): 74. doi: 10.1186/s12920-017-0308-8
[17] Lee A, Moon BI, Kim TH. BRCA1/BRCA2 Pathogenic Variant Breast Cancer: Treatment and Prevention Strategies[J]. Ann Lab Med, 2020, 40(2): 114-121. doi: 10.3343/alm.2020.40.2.114
[18] Wang B, Cao C, Liu X, et al. BRCA1-associated protein inhibits glioma cell proliferation and migration and glioma stem cell self-renewal via the TGF-β/PI3K/AKT/mTOR signalling pathway[J].Cell Oncol (Dordr), 2020, 43(2): 223-235. doi: 10.1007/s13402-019-00482-8
[19] Li AG, Murphy EC, Culhane AC, et al. BRCA1-IRIS promotes human tumor progression through PTEN blockade and HIF-1α activation[J]. Proc Natl Acad Sci U S A, 2018, 115(41):E9600-E9609. doi: 10.1073/pnas.1807112115
[20] Sun X, Cui F, Yin H, et al. Association between EGFR mutation and expression of BRCA1 and RAP80 in non-small cell lung cancer[J].Oncol Lett, 2018, 16(2): 2201-2206.
[21] Leng XF, Chen MW, Xian L, et al. Combined analysis of mRNA expression of ERCC1, BAG-1, BRCA1, RRM1 and TUBB3 to predict prognosis in patients with non-small cell lung cancer who received adjuvant chemotherapy[J]. J Exp Clin Cancer Res, 2012, 31(1): 25. doi: 10.1186/1756-9966-31-25
[22] Wood K, Hensing T, Malik R, et al. Prognostic and Predictive Value in KRAS in Non-Small-Cell Lung Cancer: A Review[J]. JAMA Oncol, 2016, 2(6): 805-812. doi: 10.1001/jamaoncol.2016.0405



 下载:
下载: