-
摘要:目的
探讨阿帕替尼治疗晚期难治性乳腺癌的临床疗效及安全性。
方法回顾性分析经多线治疗失败的晚期难治性乳腺癌患者29例,给予患者阿帕替尼500 mg/d,餐后半小时口服。观察临床疗效及不良反应发生情况。当出现Ⅲ级或以上不良反应时给予对症治疗及护理,仍不缓解时暂停用药,待不良反应恢复到≤Ⅰ级,再次应用阿帕替尼,并降低剂量为250 mg/d。
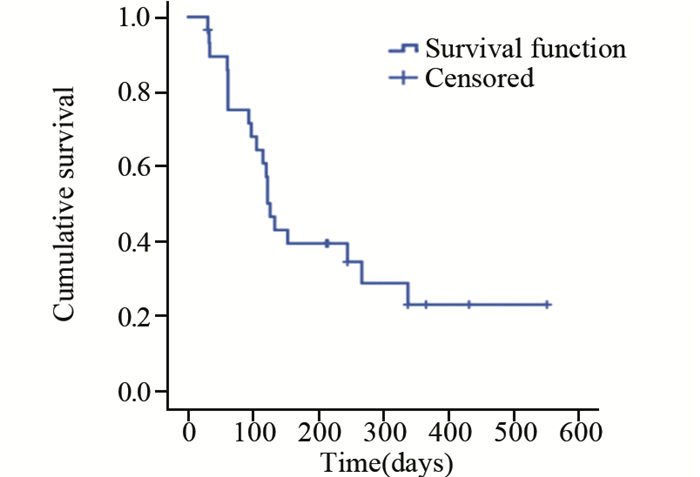
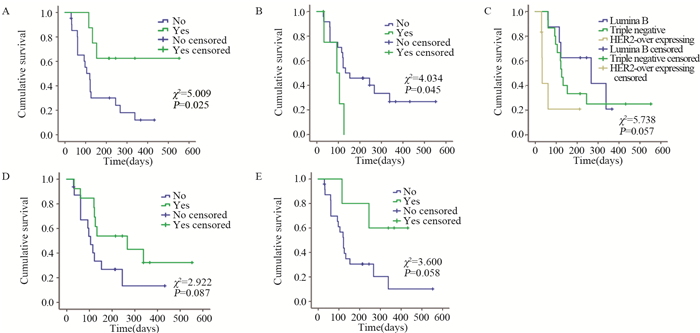
结果CR 0例,PR 37.9%(11/29),SD 44.8%(13/29),PD 17.2%(5/29),疾病控制率(PR+SD)82.8%(24/29)。中位无进展生存期126天。主要不良反应为继发性高血压(27.59%)、手足综合征(20.69%)、继发性蛋白尿(17.24%)、恶心乏力(13.79%)、继发性口腔黏膜炎(17.24%)及腹泻(10.34%),并且Ⅰ~Ⅱ级为主。Log rank单因素分析显示:在晚期难治性乳腺癌中Luminal B型(HER2阴性)及三阴性较HER2阳性型更能从阿帕替尼获益,mPFS分别为:267、126、33 d(P=0.057)。继发性高血压及继发性蛋白尿的患者mPFS更长。Cox回归分析显示:分子分型、继发高血压和继发性蛋白尿是阿帕替尼治疗晚期难治性乳腺癌mPFS的独立影响因素。
结论阿帕替尼治疗晚期难治性Luminal B(HER2阴性)型及三阴性乳腺癌仍有较好的疾病控制率及无进展生存期,不良反应可控。
Abstract:ObjectiveTo evaluate the clinical efficacy and safety of apatinib in the treatment of advanced breast cancer(ABC) patients refractory to multiline treatments.
MethodsWe retrospectively analyzed the clinical data of 29 ABC patients after the failure of multi-line treatments. Patients were treated with apatinib 500 mg/d orally. The clinical efficacy and adverse effects were evaluated. Symptomatic treatment and nursing care were given when the adverse effects were ≥grade Ⅲ and apatinib was suspended if not get relieved. When the adverse effects were ≤gradeⅠ, apatinib was administrated with reduced dosage of 250mg/d.
ResultsAmong 29 patients, there was no case with complete remission, 11(37.9%) patients with partial remission (PR), 13(44.8%) cases with stable disease (SD) and 5(17.2%) patients with progressive disease (PD). The disease control rate (PR+SD) was 82.8% (24/29). The median progression-free survival time (mPFS) was 126 days. The most common adverse effects were secondary hypertension(27.59%), hand-foot syndrome(20.69%), Secondary proteinuria(17.24%), nausea and fatigue(13.79%), Secondary oral mucositis(17.24%) and diarrhea(10.24%). Most of the side effects were degreeⅠ-Ⅱ. Log-rank univariate analysis showed a mPFS of 267 days for Luminal B(HER2-) ABC patients and 126 days for triple-negative group, compared with 33 days for HER2+ ABC patients (P=0.057). Patients with secondary hypertension or transient proteinuria had significantly longer mPFS than those without these adverse effects (P=0.025, P=0.058). Cox regression analysis identified molecular typing, secondary hypertension and proteinuria as the independent influence factors for mPFS of ABC patients treated with apatinib.
ConclusionApatinib has relatively high DCR and PFS in the treatment of Luminal B (HER2-) and triple-negative MBC patients, and adverse reactions could be controlled.
-
Key words:
- Breast cancer /
- Molecular typing /
- Apatinib /
- Clinical efficacy /
- Adverse effect
-
0 引言
甲状腺癌是人类内分泌系统和头颈部最常见的恶性肿瘤之一,其发病率在国内外均呈上升趋势[1]。许多危险因素与甲状腺癌的发病相关,包括电离辐射、雌激素、碘摄入和遗传因素等。研究表明,手术联合放化疗以及分子靶向治疗有助于控制甲状腺癌进展,延长患者的无进展生存期,提高总体生存率[2-4]。然而由于早期缺乏典型的临床表现,甲状腺癌很容易被患者自身忽略,从而错过最佳治疗时间[5]。分化型甲状腺癌一般预后较好,但当其失分化为碘难治性甲状腺癌时便进展迅速,病死率较高,预后较差[6]。乳头状甲状腺癌(papillary thyroid carcinoma, PTC)是最常见的甲状腺恶性肿瘤,约占甲状腺癌的80%[7]。据报道,在发达国家PTC的发病率呈上升趋势[8-10],PTC的不良预后因素包括年龄、性别、肿瘤大小等[7]。Grogan等[11]对269例PTC患者进行平均27年的长期随访,结果发现超过25%的患者复发,并且在11%的病例中,PTC复发发生在治疗后20多年。因此,评估患者的疾病进展情况,寻找影响PTC患者预后的相关因素值得重视[12]。
微小RNA(miRNA)是一类短的非编码RNA分子,仅含有19~22个核苷酸。它们是高度保守的分子,通过以完全或不完全互补的方式与靶基因的3’端非翻译区(3’-UTR)结合,参与靶基因的调节[13]。越来越多的研究证实,miRNA广泛参与人类癌症的发生和进展,包括甲状腺癌。miRNA在肿瘤发生和发展过程中参与细胞增殖、凋亡和肿瘤侵袭等多种恶性生物学行为[14]。虽有研究报道某些miRNA可以作为PTC的分子标志物,但目前仍缺乏敏感的miRNA组合标志物以评估PTC患者的预后。因此,本研究通过使用TCGA数据库,结合生物信息学分析对PTC组织中差异表达的miRNA进行筛选,利用Cox和Lasso回归分析出与PTC患者预后相关的miRNA,构建基于miRNA表达的预测PTC患者预后的生存模型。
1 资料与方法
1.1 原始数据的下载与处理
在TCGA官方网站上下载PTC患者的miRNA测序数据和患者的临床数据。其中癌组织514例,正常甲状腺组织59例。使用Perl5.24.3软件将原始miRNA测序数据转换成miRNA表达矩阵。在分析过程中,若有多个探针检测同一miRNA表达量,则取该miRNA表达量的平均值作为该miRNA的表达值。对于患者临床资料的分析,删除生存时间未知和生存时间为0的患者临床信息。
1.2 差异miRNA的筛选
以|log foldchange|≥2,错误发现率FDR < 0.05为筛选条件,使用R3.6.0软件中的edgeR包筛选出在甲状腺癌中差异表达的miRNA。使用ggplot2和heatmap软件程序包绘制差异基因的火山图和热图。
1.3 Cox/Lasso回归分析
结合患者的生存信息,首先对上述得到的差异miRNA进行单因素Cox回归分析,计算每个miRNA与甲状腺癌患者生存的风险比(hazard ratio, HR)和P值,以P < 0.05的标准筛选出与甲状腺癌患者预后显著相关的miRNA。将这些miRNA进一步行Lasso回归分析,目的减少基因之间共线性的影响,防止后续构建的风险模型变量过度拟合。Lasso回归使用交叉验证以确定参数,得到合适的模型。再将Lasso回归得到的miRNA进行多因素Cox回归分析,计算每个miRNA的多因素回归系数,构建风险评分方程。
1.4 风险预后模型的建立与分析
根据上述多因素Cox回归分析的结果,构建基于miRNA表达的风险评分方程risk score。按照文献报道使用公式:Risk score=β1×miRNA1EXP+β2×miRNA2EXP+......+βn×miRNAnEXP [15-16]。式中β为相应miRNA的多因素回归系数,miRNAEXP为相应miRNA的表达量。根据risk score数值的中位值,将PTC患者分为高风险评分组和低风险评分组。利用R3.6.0软件绘制模型预测预后的列线图,并比较两组患者之间生存的差异。利用R3.6.0软件绘制模型的ROC曲线和校准曲线以评价模型的敏感度和特异性。使用Survival ROC软件程序包计算受试者工作特征曲线(ROC)下面积(AUC)的数值。
2 结果
2.1 差异miRNA的筛选
利用|logfoldchange|≥2,FDR < 0.05为筛选条件,在PTC组织中共筛选到差异表达的miRNA75个。其中,上调表达的有70个、下调表达的有5个。根据FDR数值的排序前十位差异表达的miRNA,见表 1。图 1为差异miRNA相应的火山图和热图。图中红色表示与正常甲状腺组织相比,该基因在PTC组织中表达上调;绿色表示与正常甲状腺组织相比,该基因在PTC组织中表达下调。
表 1 PTC组织中前十位差异表达的miRNATable 1 Top 10 differentially-expressed miRNA in papillary thyroid carcinoma (PTC) tissues
2.2 Cox/Lasso回归分析
对上述差异表达的miRNA进行单因素Cox回归分析,计算相应miRNA与甲状腺癌患者的HR和P值,结果共有9个miRNA与甲状腺癌患者生存相关(P < 0.05):hsa-mir-6730、hsa-mir-4709、hsa-mir-196a-2、hsa-mir-146b、hsa-mir-6860、hsa-mir-509-3、hsa-mir-513c、hsa-mir-515-1、hsa-mir-551b。进一步使用lasso回归对这些miRNA进行筛选,见图 2A,并使用交叉验证建立模型,见图 2B。结果共有8个miRNA(hsa-mir-6730, hsa-mir-4709, hsa-mir-196a-2, hsa-mir-146b, hsa-mir-6860, hsa-mir-509-3, hsa-mir-513c, hsa-mir-515-1)纳入分析模型。
![]() 图 2 Lasso回归分析筛选miRNA(A)和交叉验证结果(B)Figure 2 miRNA screened by Lasso regression analysis(A) and cross validation results(B)A: the Lasso regression model and cross validation method were utilized to screen miRNA. When the number of variables was 8, the partial likelihood deviation was the minimum, corresponding to the minimum λ value; B: the regression coefficient map of miRNA in lasso model, and double dashed lines showed the 1-fold standard error of the minimum partial likelihood deviation.
图 2 Lasso回归分析筛选miRNA(A)和交叉验证结果(B)Figure 2 miRNA screened by Lasso regression analysis(A) and cross validation results(B)A: the Lasso regression model and cross validation method were utilized to screen miRNA. When the number of variables was 8, the partial likelihood deviation was the minimum, corresponding to the minimum λ value; B: the regression coefficient map of miRNA in lasso model, and double dashed lines showed the 1-fold standard error of the minimum partial likelihood deviation.2.3 风险评分方程的建立
对上述8个miRNA进行多因素Cox回归分析,根据相应的回归系数,建立风险评分方程。Risk score=0.41×hsa-mir-196a-2EXP–0.14×hsa-mir-146bEXP–0.22×hsa-mir-4709EXP+0.83×hsa-mir-509-3EXP –0.03×hsa-mir-513cEXP +0.36×hsa-mir-515-1EXP – 0.33×hsa-mir-6730EXP –0.63×hsa-mir-6860 EXP。根据此方程,计算每位甲状腺癌患者的risk score数值,并根据risk score数值的中位值,将甲状腺癌患者分为高风险评分组和低风险评分组。
2.4 风险预后模型分析
根据上述结果,利用R3.6.0软件绘制基于8个miRNA的组合预测甲状腺癌患者生存的列线图,见图 3。
2.5 风险预后模型的评价
利用R3.6.0软件绘制模型的ROC曲线以评价模型的敏感度和特异性,见图 4。我们所构建的miRNA模型预测患者3年生存率和5年生存率的ROC曲线下面积数值AUC分别为0.860和0.896,这表明模型具有较好的敏感度和特异性。同时,校准曲线的结果也显示构建的模型可靠,这些结果表明我们构建的miRNA预后模型可以较准确的预测甲状腺癌患者的生存,见图 5。
2.6 生存分析
利用R3.6.0软件中的survival程序包分析高低风险评分组患者的生存差异,绘制生存点图,图中绿色点表示未死亡患者,红色点表示死亡患者。随着risk score数值的升高,高风险评分组患者的死亡人数显著多于低风险评分组,说明高风险评分组的患者生存率较差,见图 6。
![]() 图 6 高低风险评分组患者的生存点图Figure 6 Survival points diagram of patients in high and low risk groupsThe green dots in the figure represented the surviving PTC patients, and the red dots represented the dead PTC patients. The dotted line represented the median value of risk score. The left side of the dotted line represented the low risk score group, and the right side of the dotted line represented the high risk score group. With the increase of risk score in PTC patients, the number of red dots increased gradually, and the number of dead PTC patients increased. It showed that the high risk group had poorer survival and higher risk of death.
图 6 高低风险评分组患者的生存点图Figure 6 Survival points diagram of patients in high and low risk groupsThe green dots in the figure represented the surviving PTC patients, and the red dots represented the dead PTC patients. The dotted line represented the median value of risk score. The left side of the dotted line represented the low risk score group, and the right side of the dotted line represented the high risk score group. With the increase of risk score in PTC patients, the number of red dots increased gradually, and the number of dead PTC patients increased. It showed that the high risk group had poorer survival and higher risk of death.3 讨论
甲状腺癌是最常见的内分泌恶性肿瘤。大多数甲状腺癌起源于甲状腺滤泡细胞。甲状腺癌可分为乳头状癌(75%~80%)、滤泡状癌(10%~15%)、甲状腺未分化癌(0.2%~2%)和由滤泡旁C细胞来源的髓样甲状腺癌(5%~10%)[17]。许多研究表明,miRNA与甲状腺癌的发生和进展有关。Yue等[18]研究表明,miR-7可能通过p21活化激酶1(PAK1)调节甲状腺癌细胞的生长、迁移和侵袭;Wang等[19]研究表明,碘可以通过下调miR-422a、上调MAPK1的表达,促进甲状腺癌的发生;Dong等[20]研究发现miR-141可以通过调控胰岛素受体底物2(IRS2)调控甲状腺癌细胞生长和转移,提示miR-141可以作为治疗甲状腺癌患者的潜在分子靶点;此外,miR-497也被认为是一种通过抑制脑源性神经营养因子发挥作用的甲状腺癌肿瘤抑制因子[21]。因此,miRNA可以作为甲状腺癌诊断、治疗或者预后的标志物。
本研究中,我们通过TCGA数据库构建了基于8个miRNA表达的组合预测甲状腺癌患者预后的风险模型。在这8个miRNA中,有7个miRNA被报道与甲状腺癌或者其他肿瘤相关。MiR-146b被证明在乳头状甲状腺癌中表达上调,并且与肿瘤的侵袭有关[22-23];Fu等[24]利用生物信息学的方法挖掘TCGA数据库发现hsa-mir-196a-2在甲状腺癌中表达显著上调,其与肿瘤进展、淋巴结转移和局部浸润有关,并且可以作为甲状腺癌的独立预后危险因素;miR-509的过表达可以抑制三阴性乳腺癌Hs578T细胞增殖、诱导细胞凋亡和抑制细胞侵袭[25];Tang等[26]利用生物信息学分析发现,miR-6860和miR-509-3与甲状腺癌患者的总体生存率相关,可作为甲状腺癌的预后因子;miR-513c被证明与神经母细胞瘤[27]、肝细胞癌[28]的细胞迁移、入侵和增殖等有关;has-mir-4709被证明与结肠癌[29]、胰腺导管腺癌[30]患者的生存相关。
综上所述,我们构建了基于8个miRNA预测甲状腺癌患者生存的风险模型,该模型具较好的敏感度和特异性,模型中高风险评分组患者的死亡风险较大。研究指出[31],建立多基因预后模型比患者的临床病理指标更能提供精确的预后指导,对个体化治疗方案的选择具有重要的参考价值。我们所构建的8个miRNA模型可有效预测甲状腺癌患者的预后,但仍需要进一步使用大规模的多中心的循证医学证据加以验证。
Competing interests: The authors declare that they have no competing interests.作者贡献王静:病例资料收集,数据整理及分析、论文撰写及修改贾敬好:课题构思指导,论文指导及修改刘晶晶:临床资料整理及随访崔志超:临床病例资料收集熊伟、王晓红:课题构思指导 -
表 1 29例晚期难治性乳腺癌患者一般资料
Table 1 Clinical characteristics of 29 advanced breast cancer patients

表 2 阿帕替尼治疗ABC患者预后的单因素分析
Table 2 Univariate analysis of prognosis of ABC patients treated with apatinib

表 3 阿帕替尼治疗ABC患者预后的多因素分析结果
Table 3 Multivariable analysis of prognosis of ABC patients treated with apatinib

表 4 阿帕替尼主要相关不良反应发生情况(n(%))
Table 4 Incidence of main adverse effects related to apatinib (n(%))

-
[1] Cardoso F, Harbeck N, Fallowfield L, et al. Locally recurrent or metastatic breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2012, 23 suppl 7: vii 11-19.
[2] Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis[J]. Nature, 2011, 473(7347): 298-307. doi: 10.1038/nature10144
[3] Huang L, Wei Y, Shen S, et al. Therapeutic effect of apatinib on overall survival is mediated by prolonged progression-free survival in advanced gastric cancer patients[J]. Oncotarget, 2017, 8(17): 29346-20354. doi: 10.18632/oncotarget.12897
[4] Jain RK. Antiangiogenesis strategies revisited: from starving tumors to alleviating hypoxia[J]. Cancer Cell, 2014, 26(5): 605-622. doi: 10.1016/j.ccell.2014.10.006
[5] Li J, Zhao X, Chen L, et al. Safety and pharmacokinetics of novel selective vascular endothelial growth factor receptor-2 inhibitor YN968D1 in patients with advanced malignancies[J]. BMC Cancer, 2010, 10: 529. doi: 10.1186/1471-2407-10-529
[6] Anderson BO, Shyyan R, Eniu A, et al. Breast cancer in limited-resource countries: an overview of the breast health global initiative 2005 guidelines[J]. Breast J, 2006, 12 Suppl 1: S3-S15. http://europepmc.org/abstract/MED/16430397
[7] Verheul HMW, Voest EE, Schlingemann RO. Are tumours angiogenesis-dependent?[J]. J Pathol, 2004, 202(1): 5-13. doi: 10.1002/path.1473
[8] Rossari JR, Metzger-Filho O, Paesmans M, et al. Bevacizumab and Breast Cancer: A Meta-Analysis of First-Line Phase Ⅲ Studies and a Critical Reappraisal of Available Evidence[J]. J Oncol, 2012, 2012: 417673. http://www.ncbi.nlm.nih.gov/pubmed/23008712
[9] Vrdoljak E, Marschner N, Zielinski C, et al. Final results of the TANIA randomised phase Ⅲ trial of bevacizumab after progression on first-line bevacizumab therapy for HER2-negative locally recurrent/metastatic breast cancer[J]. Ann Oncol, 2016, 27(11): 2046-2052. doi: 10.1093/annonc/mdw316
[10] Drooger JC, van Tinteren H, de Groot SM, et al. A randomized phase 2 study exploring the role of bevacizumab and a chemotherapy-free approach in HER2-positive metastatic breast cancer: The HAT study (BOOG 2008-2003), a Dutch Breast Cancer Research Group trial[J]. Cancer, 2016, 122(19): 2961-2970. doi: 10.1002/cncr.30141
[11] Martín M, Loibl S, Hyslop T, et al. Evaluating the addition of bevacizumab to endocrine therapy as first-line treatment for hormone receptor-positive metastatic breast cancer: a pooled analysis from the LEA (GEICAM/2006-11_GBG51) and CALGB 40503 (Alliance) trials[J]. Eur J Cancer, 2019, 117: 91-98. doi: 10.1016/j.ejca.2019.06.002
[12] 张化芝, 李晓双, 郭晓烨, 等.阿帕替尼通过抑制糖酵解途径对乳腺癌MDA-MB-231细胞增殖抑制及凋亡的作用[J].肿瘤防治研究, 2019, 46(5): 401-405. doi: 10.3971/j.issn.1000-8578.2019.18.1422 Zhang HZ, Li XS, Guo XY, et al. Apatinib Suppresses Proliferation and Induced Apoptosis of Human Breast Cancer Cell Line MDA-MB-231 Through Glycolytic Inhibition[J]. Zhong Liu Fang Zhi Yan Jiu, 2019, 46(5): 401-405. doi: 10.3971/j.issn.1000-8578.2019.18.1422
[13] Gao Z, Shi M, Wang Y, et al. Apatinib enhanced anti-tumor activity of cisplatin on triple-negative breast cancer through inhibition of VEGFR-2[J]. Pathol Res Pract, 2019, 215(7): 152422. doi: 10.1016/j.prp.2019.04.014
[14] Hu X, Zhang J, Xu B, et al. Multicenter phase Ⅱ study of apatinib, a novel VEGFR inhibitor in heavily pretreated patients with metastatic triple-negative breast cancer[J]. Int J Cancer, 2014, 135(8): 1961-1969. doi: 10.1002/ijc.28829
[15] Hu X, Cao J, Hu W, et al. Multicenter phase Ⅱ study of apatinib in non-triple-negative metastatic breast cancer[J]. BMC Cancer, 2014, 14: 820. doi: 10.1186/1471-2407-14-820
[16] Lin Y, Wu Z, Zhang J, et al. Apatinib for metastatic breast cancer in non-clinical trial setting: Satisfying efficacy regardless of previous anti-angiogenic treatment[J]. Tumour Biol, 2017, 39(6): 1010428317711033. http://europepmc.org/abstract/MED/28639910
[17] Zhu A, Yuan P, Wang J, et al. Apatinib combined with chemotherapy in patients with previously treated advanced breast cancer: An observational study[J]. Oncol Lett, 2019, 17(6): 4768-4778. http://www.researchgate.net/publication/332165686_Apatinib_combined_with_chemotherapy_in_patients_with_previously_treated_advanced_breast_cancer_An_observational_study
[18] Li Y, Zhou Y, Wang Y, et al. Comparison of apatinib and capecitabine (Xeloda) with capecitabine (Xeloda) in advanced triple negative breast cancer as third-line therapy A retrospective study[J]. Medicine (Baltimore), 2018, 97(36): e12222. doi: 10.1097/MD.0000000000012222
[19] 秦叔逵, 李进.阿帕替尼治疗胃癌的临床应用专家共识[J].临床肿瘤学杂志, 2015, 20(9): 841-847. http://www.cnki.com.cn/Article/CJFDTotal-LCZL201509014.htm Qin SQ, Li J. Expert consensus on the clinical application of apatinib for gastric cancer[J]. Lin Chuang Zhong Liu Xue Za Zhi, 2015, 20(9): 841-847. http://www.cnki.com.cn/Article/CJFDTotal-LCZL201509014.htm
[20] Sun D, Hou H, Zhang C, et al. The efficacy and safety of apatinib for refractory malignancies: a review and meta-analysis[J]. Onco Targets Ther, 2018, 11: 6539-6554. doi: 10.2147/OTT.S176429
[21] Fan M, Zhang J, Wang Z, et al. Phosphorylated VEGFR2 and hypertension: potential biomarkers to indicate VEGFdependency of advanced breast cancer in anti-angiogenic therapy[J]. Breast Cancer Res Treat, 2014, 143(1): 141-151. doi: 10.1007/s10549-013-2793-6
-
期刊类型引用(0)
其他类型引用(1)



 下载:
下载: