Surgery and Neoadjuvant Chemotherapy After Surgery on Surgical-pathologic Staging in Clinical ⅠB-ⅡB Period Cervical Cancer Patients
-
摘要:目的
探讨临床分期及手术-病理分期在临床ⅠB~ⅡB期宫颈癌诊治中的意义。
方法回顾性分析行手术治疗的388例ⅠB~ⅡB期宫颈癌患者的临床病理资料,分为直接手术(DS)和术前新辅助化疗(NACT)组,观察两组临床分期与手术-病理分期的差异。
结果临床分期与手术-病理分期符合率为:DS组21.1%,NACT组10%。临床检查对阴道及宫旁浸润判断的敏感度、特异性、准确度DS和NACT组分别为66.7%、20.0%,67.5%、70.9%,67.4%、69.7%和50.0%、85.7%,58.0%、46.0%,57.6%、47.6%。DS组不同分期的阴道、深肌层浸润差异有统计学意义(P < 0.05)。DS组以pTNM进行分期,癌栓是影响预后的因素(DFS: P=0.013, OS: P=0.004);以FIGO分期,分期与预后密切相关(DFS: P=0.024, OS: P=0.050)。NACT组FIGO分期中的分期是影响复发的因素(P=0.023),而淋巴结转移与预后密切相关(DFS: P=0.004, OS: P=0.044)。
结论手术-病理分期与临床分期在ⅠB~ⅡB期宫颈癌中存在明显差异,其中ⅡB期的误差率最高,分期偏高导致本可手术的患者失去手术机会。
Abstract:ObjectiveTo discuss the feasibility and importance of clinical staging and surgical-pathological staging in the treatment on stagesⅠB-ⅡB cervical cancer.
MethodsWe retrospectively analyzed the clinicopathological data of 388 patients with stagesⅠB-ⅡB cervical cancer who accepted surgical treatment. These patients were divided into preoperative neoadjuvant chemotherapy group (NACT group) and direct surgery group (DS group). The differences of the results were observed.
ResultsFor surgical-pathological and clinical staging, the total coincidence rates were 21.1% in DS groups and 10% in NACT groups. For vaginal invasion, the sensitivity, specificity and accuracy were 66.7%, 67.5%, 67.4% in DS group and 50.0%, 58.0%, 57.6% and in NACT group; For parametrial invasion, the sensitivity, specificity and accuracy were 20.0%, 70.9%, 69.7% in DS group and 85.7%, 46.0%, 47.6% in NACT group respectively. The deep stromal invasion and vaginal invasion showed the distinct difference between each stage in DS group(P < 0.05). Tumor emboli could affect the prognosis in pTNM staging of DS group (DFS: P=0.013, OS: P=0.004); but in FIGO staging, staging was closely related to the prognosis (DFS: P=0.024, OS: P=0.050). In NACT group, the staging affected the recurrence(P=0.023), while lymph node metastasis was closely related to the prognosis (DFS: P=0.004, OS: P=0.044).
ConclusionWith an obvious difference between surgical-pathological and clinical staging in stagesⅠB-ⅡB cervical cancer. There is a high percentage of discrepancy in clinical stage ⅡB. Due to the over-staging, many patients in clinical stage ⅡB lose the opportunities of surgery.
-
Key words:
- Cervical carcinoma /
- FIGO staging /
- Surgical-pathological staging /
- Prognosis
-
0 引言
宫颈癌是女性,特别是发展中国家女性的常见生殖系统疾病之一,位居全世界常见女性肿瘤的第二位[1],且近年来其发病率有年轻化趋势[2]。虽然经近20年的宫颈癌筛查工作的开展及治疗水平的提高,宫颈癌的发病率在下降,生存率在提高,但是仍不理想,宫颈癌的临床诊治水平如何提高仍有待进一步探讨。
宫颈癌临床分期采用的是国际妇产科联盟(international federation of gynecology and obste-trics, FIGO)的标准。根据FIGO分期,ⅠA期患者主要依靠组织病理进行确诊;而ⅠB~ⅡB期患者主要依靠妇科检查了解阴道或宫旁组织的受侵程度进行判断。由于检查方法的局限性及检查者的主观因素影响,对宫旁浸润的判断是目前临床分期的难点,易导致ⅠB~ⅡB期患者的临床分期与手术-病理分期(pTNM)的不相符,且宫颈癌临床分期未纳入淋巴结转移、深间质浸润、淋巴血管间隙受侵、病理类型、组织分化等预后有关的危险因素。因此仍存在局限性。
近年来,有学者建议将pTNM分期作为宫颈癌新的分期[3]。为宫颈癌的治疗提供更加全面客观的依据,使治疗更加科学,从而提高预后。本研究探讨临床分期存在的问题,pTNM分期的可行性及重要性。并且将宫颈癌直接手术与术前新辅助化疗组对比,探讨新辅助化疗对pTNM分期的影响。
1 资料与方法
1.1 研究对象
选择2007年1月—2013年3月广西医科大学附属肿瘤医院初次收治的,经组织病理学确诊为宫颈癌的,行手术治疗的ⅠB~ⅡB期宫颈癌患者共388例,其中直接手术(DS组)218例,新辅助化疗后行手术治疗(NACT组)170例,纳入标准如下:(1)术前活体组织病理学检查诊断为原发性宫颈癌,临床分期为ⅠB~ⅡB(排除复发癌及转移癌);(2)术前无任何辅助治疗或仅行新辅助化疗;(3)全部病例均行开腹或腹腔镜下广泛全子宫(Ⅲ型)+盆腔±腹主动脉旁淋巴结清扫±双侧附件切除,要求保留卵巢且术中卵巢外观正常者可保留双侧卵巢,行脐水平以上结肠旁沟卵巢移位术;(4)有术后手术病理标本检查结果;(5)临床病例资料完整。
1.2 研究方法
分别对DS与NACT组临床分期及pTNM分期的病理类型、组织学分级、阴道浸润、宫旁浸润、期别相符性进行比较,比较两组分期与预后因素的关系及生存率,并对两组的各种预后相关因素进行分层分析。
1.2.1 分期标准
按照FIGO2009年修订的宫颈癌临床分期系统[4],对所有病例进行术前临床分期。术后根据术中大体病理及术后病理结果,按照美国癌症联合委员会(AJCC)制定的pTNM分期标准[3]对上述病例重新进行分期。
1.2.2 纳入患者的基本情况
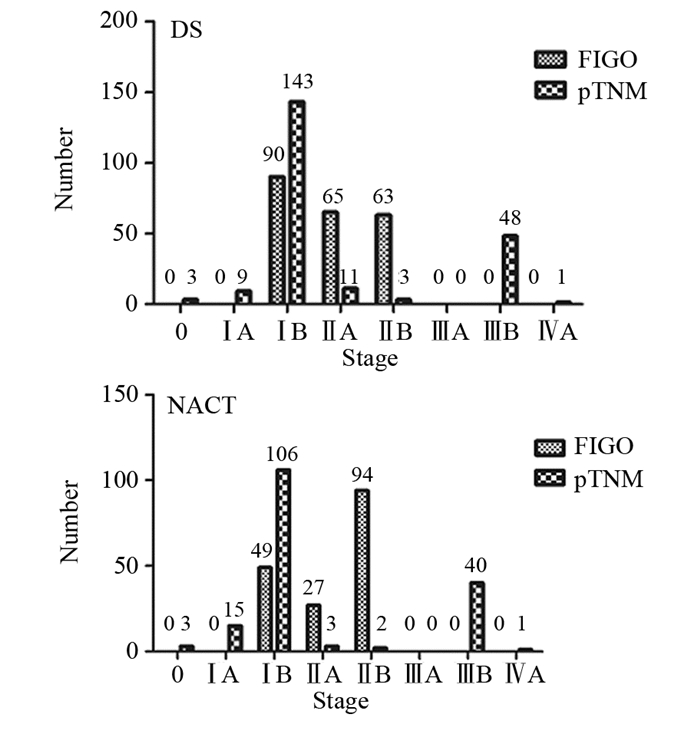
DS组:中位年龄为46.0岁(21~72岁),ⅠB期90例,ⅡA期65例,ⅡB期63例;组织分级G1级14例,G2级38例,G3级163例,有3例术前未描述分化;鳞癌167例,腺癌28例,腺鳞癌18例,其他5例。
NACT组中:中位年龄为48.0(26~71岁),ⅠB期49例,ⅡA期27例,ⅡB期94例;组织学分级G1级10例,G2级38例,G3级121例,1例未分化;鳞癌115例,腺癌26例,腺鳞癌14例,其他15例。
1.3 随访方法
先与患者取得联系,经患者同意后将调查表寄到患者家中,由患者本人填写调查表后再寄回。如不方便邮寄调查表者进行电话问卷调查。截止时间为患者死亡或截至2014年10月30日,并计算累积5年总生存率(OS)及5年无瘤生存率(DFS)。
1.4 统计学方法
用SPSS16.0软件包进行统计学分析,计数资料进行χ2检验,采Kaplan-Meier法计算生存率,Stata11.0软件进行分层分析、生存率诊断比值比及95%CI分析,P < 0.05为差异有统计学意义。
2 结果
2.1 纳入患者分期情况
纳入患者手术前和手术后分期情况,见表 1~2。DS组与NACT组中的FIGO分期与pTNM分期的分期情况,见图 1。
表 1 ⅠB~ⅡB期宫颈癌患者DS组FIGO分期与pTNM分期的比较Table 1 Comparison between FIGO staging and pTNM staging in DS group of clinicalⅠB-ⅡB period cervical cancer patients 表 2 ⅠB~ⅡB期宫颈癌患者NACT组FIGO分期与pTNM分期的比较Table 2 Comparison between FIGO staging and pTNM staging in NACT group of clinicalⅠB-ⅡB period cervical cancer patients
表 2 ⅠB~ⅡB期宫颈癌患者NACT组FIGO分期与pTNM分期的比较Table 2 Comparison between FIGO staging and pTNM staging in NACT group of clinicalⅠB-ⅡB period cervical cancer patients
2.2 病理类型
DS组:手术前后病理类型依次为:鳞癌167例和163例,腺癌28例和25例,腺鳞癌18例和2例,其他5例和8例,误差率分别为8.4%、14.3%、50.0%、40.0%,总误差率为13.3%。NACT组:手术前后病理类型依次为:鳞癌115例和103例,腺癌26例和23例,腺鳞癌14例和26例,其他15例和18例,误差率分别为15.7%、19.2%、21.4%、6.7%,总误差率为15.9%。
2.3 组织学分级
DS组:手术后组织学分级:G1级12例,G2级32例,G3级159例,15例未计(3例术后为CIN3,1例术前未描述,12例术后未描述),误差率分别为27.2%、50.0%、8.3%,总误差率为16.7%。NACT组:手术后组织学分级:G1级10例,G2级30例,G3级126例,4例未计(1例术后为未分化,3例术后为CIN3),误差率分别为33.3%、42.1%、6.7%,总误差率为16.3%。
2.4 手术前后分期的改变
DS组及NACT组的分期前后比较显示,FIGO同一分期均比pTNM分期偏高,提示FIGO分期的客观评价存在较大误差,见表 1~2。
2.5 临床检查对阴道浸润的判断
DS组:手术前76例存在阴道受侵,术后其符合仅为10例;手术前142例无阴道受侵,术后其符合为137例。敏感度66.7%(漏诊率33.3%),特异性67.5%(误诊率32.5%)。阳性、阴性预测值分别为13.2%、96.5%。两种检查的一致率(准确度)为67.4%。
NACT组:手术前72例存在阴道受侵,术后发现其符合仅为4例;手术前98例无阴道受侵,术后发现其符合为94例。敏感度50.0%(漏诊率50.0%),特异性58.0%(误诊率42.0%)。阳性、阴性预测值分别为5.6%、96.0%。两种检查的一致率(准确度)为57.6%。
2.6 临床检查对宫旁浸润的判断
DS组:手术前63例存在宫旁浸润,术后发现其符合仅为1例;手术前155例无宫旁浸润,术后发现其符合为151例。敏感度20.0%(漏诊率80.0%),特异性70.9%(误诊率29.1%)。阳性、阴性预测值分别为1.6%、97.4%。两种检查的一致率(准确度)为69.7%。
NACT组:手术前94例存在宫旁浸润,术后其符合仅为6例;手术前76例无宫旁浸润,术后发现其符合为75例。敏感度85.7%(漏诊率14.3%),特异性46.0%(误诊率54.0%)。阳性、阴性预测值分别为6.4%、98.7%。两种检查的一致率(准确度)为47.6%。
2.7 FIGO分期与预后相关因素的关系
DS组:ⅠB期患者中,宫旁受侵2例,累及阴道1例,癌栓19例,深肌层受侵53例,淋巴结转移18例;ⅡA期患者中,宫旁受侵1例,累及阴道8例,癌栓17例,深肌层受侵41例,淋巴结转移16例;ⅡB期患者中,宫旁受侵1例,累及阴道6例,癌栓10例,深肌层受侵49例,淋巴结转移16例,盆腔转移1例。
NACT组:ⅠB期患者中,癌栓4例,深肌层受侵27例,淋巴结转移10例,盆腔转移1例;ⅡA期患者中,宫旁受侵1例,累及阴道1例,癌栓4例,深肌层受侵17例,淋巴结转移9例,盆腔转移1例;ⅡB期患者中,宫旁受侵6例,累及阴道7例,癌栓9例,深肌层受侵47例,淋巴结转移22例,盆腔转移2例。
2.8 生存分析
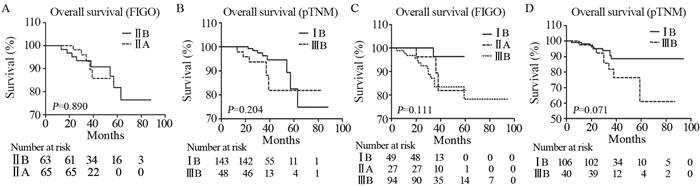
DS组中,失访13例,死亡12例,中位随访时间为,34.0月(13~88月),按照FIGO临床分期,其5年生存率分别为:ⅠB期100%,ⅡA期93.8%,ⅡB期88.6%。ⅡA期与ⅡB期生存率比较,差异无统计学意义(P=0.890);按照pTNM分期,0、ⅠA、ⅡA、ⅡB和ⅣA期例数少,未发现死亡患者,ⅠB期及ⅢB期5年生存率分别为95.0%、89.6%,差异无统计学意义(P=0.204)。
NACT组中,失访15例,死亡18例,中位随访时间为,35.0月(4~94月),按照FIGO临床分期,其5年生存率分别为:ⅠB期95.8%,ⅡA期88.1%,ⅡB期86.0%,生存率比较差异无统计学意义(P=0.111);按照pTNM分期,0、ⅠA、ⅡA和ⅣA期例数少,未发现死亡患者。ⅡB期总共2例,死亡1例。ⅠB期及ⅢB期5年生存率分别为92.3%、79.0%,差异无统计学意义(P=0.071),见图 2。
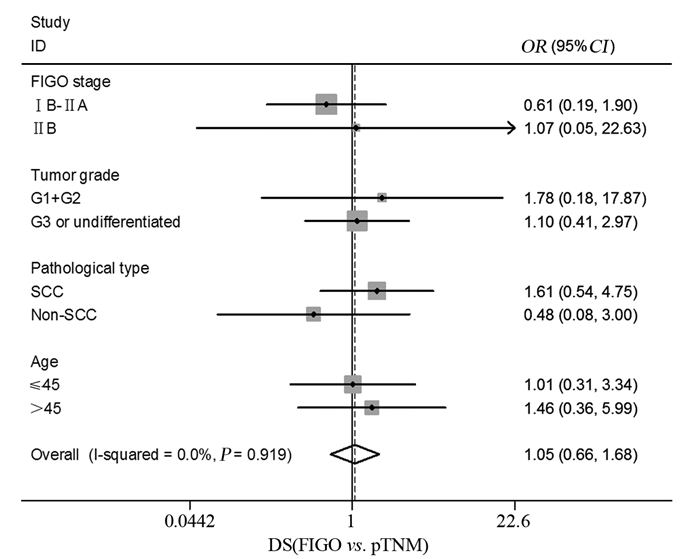
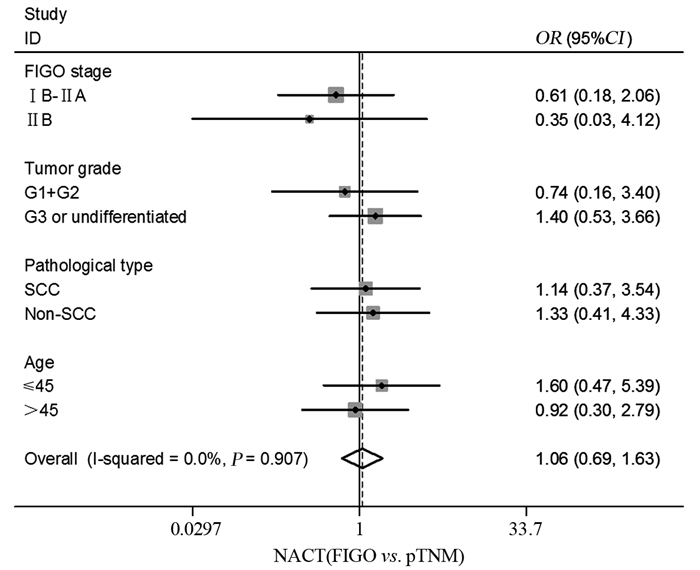
2.9 分层分析
DS组及NACT组中,对宫颈癌行FIGO分期为ⅠB~ⅡB期分及pTNM分期为ⅠB ~ⅡB期的患者进行分层分析,内容包括分期、组织分化、病理类型、年龄,结果显示DS组中,进行FIGO分期及pTNM分期,ⅠB~ⅡB期宫颈癌患者中这些因素差异无统计学意义(P > 0.05);而NACT组中两者分析这些因素差异亦无统计学意义(P > 0.05),见图 3~4。
2.10 预后分析
针对两种不同分期标准的分期、年龄、组织学分级、病理类型、淋巴结转移、深肌层浸润、癌栓、宫旁转移各因素进行预后分析,结果显示DS组:pTNM进行分期,癌栓是影响预后的因素(DFS: P=0.013, OS: P=0.004);FIGO分期中,分期与预后密切相关(DFS: P=0.024, OS: P=0.050)。NACT组:FIGO分期中的分期是影响复发的因素(P=0.023),而淋巴结转移与预后密切相关(DFS: P=0.004, OS: P=0.044)。
3 讨论
3.1 FIGO分期和pTNM分期差异的探讨
宫颈癌的临床分期存在一定的局限性,妇科医生进行双合诊及三合诊对盆腔进行检查,结合取得的病理和辅助检查作出判断,受主观因素影响较大,术前很难准确评估肿瘤浸润范围,导致诊断偏差,而且已确认的临床分期不能因为后续的临床发现改变,这也是临床分期和pTNM分期存在较大差别的原因。文献报道以手术病理分期为标准约25%FIGOⅠ~Ⅱ期、60%FIGOⅢ的患者被低估分期,因此所制定的治疗方案很可能出现过度治疗或治疗不足等得问题[5]。同时淋巴结转移[6]、深间质浸润[7]、淋巴血管间隙受侵、组织分化、病理类型等影响预后的危险因素未纳入其中。这些不足之处严重影响了治疗方案的正确选择及准确的预后评估。
近几年,越来越多的学者重视这个问题,推荐引用国际抗癌联盟(UICC)的pTNM分期系统进行宫颈癌的手术病理分期。该分期是在术前获得临床资料的基础上,结合后续的手术情况及病理结果对患者进行分期,可以更加全面和准确的评估肿瘤浸润范围,为术后辅助治疗方案的选择及预后的准确评估提供重要依据。Quinn等[8]报道了4 729例ⅠA、ⅠB、ⅡA、ⅡB期患者的FIGO与pTNM分期相符率分别为95%、83%、60%、59%,Ⅲ期的误诊率高达42.9%~89.5%。20%~30%的临床ⅡB期的患者诊断不足,而64%的ⅢB期患者分期偏高。而本研究中FIGO和pTNM分期的符合率分别为:DS组中ⅠB期65.6%,ⅡA期9.2%,ⅡB期1.6%;NACT组中ⅠB期71.4%,ⅡA期3.7%,ⅡB期2.1%,可见随着分期的升高,相符率逐渐降低,但是本研究中ⅡA、ⅡB期的相符率明显偏低。针对各期出现的差异,进行分析:ⅠB期的诊断最主要是依靠临床检查,肉眼评估肿瘤的大小,受检查者的个人经验和主观判断影响很大,而且在实际应用中,大部分患者伴随宫颈糜烂,妇检诊断ⅠB期的患者可能术中未见病灶,术后确诊CIN3或早期浸润癌的病例不少见,严重影响检查者对患者分期的判断。而这也是手术-病理分期应该用于宫颈癌的一个主要原因。病理的确定完全是根据术后,还是结合术前取病理的结果对患者下最后诊断?这有待进一步研究。本研究DS组中临床ⅠB期的有3例就出现这种情况,术后诊断为CIN3,约占3.3%。术前DS组临床分期为ⅠB期90例,术后相符率仅为65.6%(59/90),其中有24.4%(22/90)pTNM分期升高,32.2%(29/90)pTNM分期降低;NACT组临床分期ⅠB期49例,术后相符率仅为71.4%(35/49),其中有26.5%(13/49)pTNM分期升高,44.9%(22/49)pTNM分期降低。分析其原因,临床缺乏客观、有效的检查方法评估肿瘤情况,个人经验和客观影响因素起主导作用,导致pTNM分期降低;而术前无法准确评估肿瘤侵犯范围及淋巴结转移情况是导致pTNM分期升高主要原因,Monnier等[9]研究发现,无淋巴结转移的Ⅰ~Ⅱ期宫颈癌患者术后化疗有更高的5年生存率。
Ⅱ期是指肿瘤超越子宫颈,但尚未达骨盆壁或未达阴道下段1/3,ⅡA期主要依靠妇科检查的触诊及窥查判断宫旁和阴道受浸润程度。本研究发现DS组中,ⅡA期相符率仅为9.2%,ⅡB期1.6%;NACT组中ⅡA期相符率仅为3.7%,ⅡB期2.1%,部分患者因为宫旁增厚而诊断为ⅡB期,术后病理却提示CIN3,DS组中有1例,占1.6%,NACT组中有3例,占3.2%,NACT组较DS组偏高,考虑化疗后肿瘤缩小、宫旁浸润范围变小的影响。
本研究DS组中FIGO分期为ⅡA期有65例,ⅡB期有63例,因FIGO分期诊断不准确导致的误差率ⅡA期为80.8%,ⅡB期为98.4%;而NACT组中FIGOⅡA期有27例,ⅡB期有94例,因临床分期诊断不准确导致的误差率ⅡA期为96.3%,ⅡB期为97.9%。另一方面,本研究针对阴道及宫旁受浸润情况进行了术前和术后对比,结果提示:通过临床盆腔检查的阴道和宫旁受浸润相符率偏低。分析其原因如下:(1)ⅡA期患者主要靠肉眼观察穹隆变浅或消失来判定阴道是否受侵,结合肿瘤大小及在阴道所处位置来进行判定,受个人经验和主观因素影响较大;(2)ⅡB期患者临床主要靠检查者触及宫旁情况,包括主、骶韧带增厚、变硬、缩短与否进行确定。可是宫旁组织增厚混淆因素很多,比如盆腔炎性反应、个人经验、患者妇检配合程度等,这也是导致ⅡB期诊断偏高的原因。
根据2014年最新NCCN指南,临床分期为ⅡB期推荐行同步放化疗,但是放疗会导致阴道纤维化及黏连、狭窄、缩短,卵巢功能破坏,远期放射性膀胱炎和直肠炎等问题严重影响患者治疗后生活质量,尤其是性生活质量严重受损[10-11]。本研究中ⅡB期误差率最大,对宫旁浸润评估错误,导致该期临床分期偏高,使早期浸润患者失去手术机会。本研究DS组中ⅡB期47例患者诊断偏高,NACT组中70例诊断偏高,这些患者是否行手术治疗,是目前研究需进一步探讨的的问题。
3.2 新辅助化疗对pTNM分期的影响
宫颈癌行术前新辅助化疗一直是个有争论的话题,部分学者认为可减少宫颈癌复发的危险因素,但是不可提高宫颈癌患者生存率。Takatori等[12]对宫颈癌ⅡA2~ⅡB期NACT组(28例)vs. DS组(17例)进行对比研究,发现新辅助化疗组的盆腔淋巴结转移率明显小于直接手术组(P=0.001)。本研究结果显示DS组与NACT组ⅠB、ⅡA和ⅡB期符合率相比较,在各期两者差异均无统计学意义(P=0.480, P=0.632, P=1.000),总体偏低率亦无统计学意义(P=0.138, P=0.770, P=0.985),总体偏高率无差别(P=0.787, P=0.392, P=0.953)。提示NACT化疗对术后pTNM分期的正确分期无影响。
3.3 宫颈癌pTNM分期临床应用必要性
淋巴结转移是目前公认的影响预后的重要因素之一[13]。淋巴结状态对评估预后及更“个体化”治疗方案的制定有十分重要作用,宫颈癌的pTNM分期将淋巴结受累情况纳入了分期依据,补充了FIGO分期的不足。本文分层分析显示,在分期、组织分化、病理类型、年龄方面,FIGO与pTNM分期在DS组或NACT组中均无统计学意义。FIGO分期与预后存在密切关系,Andrae等[14]报道按照FIGO分期,结果显示患者5年生存率为:ⅠA期95%,ⅠB期85%,Ⅱ期54%,Ⅲ期及超过Ⅲ期22%。Quinn等[8]对宫颈癌患者按照pTNM分期,随访结果显示各期5年生存率为:ⅠA1期95.1%, ⅠA2期98.6%,ⅠB1期92.5%,ⅠB2期82.9%,ⅡA期79.9%,ⅡB期70.6%,ⅢA期58.5%,ⅢB期60.2%,ⅣA期26.4%,ⅣB期17.7%。
本研究发现,按照FIGO分期,DS组中ⅠB期100%,ⅡA期93.8%,ⅡB期88.6%;NACT组中其5年生存率分别为:ⅠB期95.8%,ⅡA期88.1%,ⅡB期86.0%。按照pTNM分期,DS组中,ⅠB期及ⅢB期5年生存率分别为95.0%、89.6%;NACT组中,ⅠB期及ⅢB期5年生存率分别为92.3%、79.0%,其余因例数过少未统计。各组间生存率差异均无统计学意义。本研究均较文献偏高,考虑与样本量偏小有关,需进一步开展大样本量研究。
但是,影响宫颈癌预后的因素还有很多,包括血管淋巴管间隙浸润、宫颈深肌层浸润、病理类型、组织学分级等。本文预后相关因素分析显示,DS组中行pTNM分期的存在癌栓患者预后更差(DFS: P=0.013, OS: P=0.004);而在NACT组中存在淋巴结转移的患者预后较差(DFS: P=0.004, OS: P=0.044)。如病理类型和组织分期在术前虽然能得到结果,但由于取样局限和取样量偏小,术前术后存在误差,且如深肌层和淋巴管间隙浸润需手术治疗后行病理检查才能发现或证实。以上因素宫颈癌pTNM分期尚未纳入其中,如何将这些影响预后的因素和宫颈癌分期更好的结合,准确的评估预后及指导术后辅助治疗的选择,从而提高宫颈癌的生存率,是一个值得进一步探讨的问题。
总之,宫颈癌临床分期存在多年,在一定程度上可以很好评估预后,但是存在主观性和个人经验主导的局限性;宫颈癌的pTNM分期是根据术后病理进行分期,更客观准确,使治疗更“个体化”,为预后的评估及辅助治疗方案的选择提供更好的依据,但是部分影响预后的危险因素尚未纳入该分期中,宫颈癌pTNM分期需进一步完善。相信随着pTNM分期的不断完善和医疗技术的发展,宫颈癌的pTNM分期可以在临床得到广泛的应用。
-
表 1 ⅠB~ⅡB期宫颈癌患者DS组FIGO分期与pTNM分期的比较
Table 1 Comparison between FIGO staging and pTNM staging in DS group of clinicalⅠB-ⅡB period cervical cancer patients

表 2 ⅠB~ⅡB期宫颈癌患者NACT组FIGO分期与pTNM分期的比较
Table 2 Comparison between FIGO staging and pTNM staging in NACT group of clinicalⅠB-ⅡB period cervical cancer patients

-
[1] Jemal A, Simard EP, Dorell C, et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV) associated cancers and HPV vaccination coverage levels[J]. J Natl Cancer Inst, 2013, 105(3): 175-201. doi: 10.1093/jnci/djs491
[2] Siegel R, Ma J, Zou Z, et al. Cancer Statistics, 2014[J]. Ca Cancer J Clin 2014, 64(1): 9-29. doi: 10.3322/caac.21208
[3] Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium[J]. Int J Gynaecol Obstet, 2009, 105(2): 103-4. doi: 10.1016/j.ijgo.2009.02.012
[4] Printz C. New AJCC cancer staging manual reflects changes in cancer knowledge[J]. Cancer, 2010, 116(1): 2-3. doi: 10.1002/cncr.v116:1
[5] Benedet JL, Bender H, Jones H, et al. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology[J]. Int J Gynaecol Obstet, 2009, 209(2): 209-62. https://www.ncbi.nlm.nih.gov/pubmed/11041682
[6] Uegaki K, Shimada M, Sato S, et al. Outcome of stage IB2-ⅡB patients with bulky uterine cervical cancer who underwent neoadjuvant chemotherapy followed by radical hysterectomy[J]. Int J Clin Oncol, 2014, 19(2): 348-53. doi: 10.1007/s10147-013-0559-0
[7] Yu Q, Lou XM, He Y. Prediction of local recurrence in cervical cancer by a Cox model comprised of lymph node status, lymph-vascularspace invasion, and intratumoral Th17 cell-infiltration[J]. Med Oncol, 2014, 31(1): 795. doi: 10.1007/s12032-013-0795-1
[8] Quinn MA, Benedef JL, Odicino F, et al. Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer[J]. Int J Gyneeol Obstet, 2006, 95(Suppl 1):S43-103. https://www.ncbi.nlm.nih.gov/pubmed/17161167
[9] Monnier L, Touboul E, Daraï E, et al. Stage IB2, ⅡA and ⅡB cervical carcinoma without lymph node extension treated with neoadjuvant chemoradiotherapy[J]. Bull Cancer, 2016, 103(2): 164-72. doi: 10.1016/j.bulcan.2015.11.010
[10] Katepratoom C, Manchana T, Amornwichet N, et al. Lower urinary tract dysfunction and quality of life in cervical cancer survivors after concurrent chemoradiation versus radical hysterectomy[J]. Int Urogynecol J, 2014, 25(1): 91-6. doi: 10.1007/s00192-013-2151-6
[11] Greimel ER, Winter R, Kapp KS, et al. Quality of life and sexual functioning after cervical cancer treatment: a long-term follow-up study[J]. Psychooncology, 2009, 18(5): 476-82. doi: 10.1002/pon.v18:5
[12] Takatori E, Shoji T, Takada A, et al. A retrospective study of neoadjuvant chemotherapy plus radical hysterectomy versus radical hysterectomy alone in patients with stage Ⅱ cervical squamous cell carcinoma presenting as a bulky mass[J]. Oncol Targets Ther, 2016, 9: 5651-7. doi: 10.2147/OTT
[13] Colturato LF, Signorini Filho RC, Fernandes RC, et al. Lymph node micrometastases in initial stage cervical cancer and tumoral recurrence[J]. Int J Gynaecol Obstet, 2016, 133(1): 69-75. doi: 10.1016/j.ijgo.2015.08.019
[14] Andrae B, Andersson TM, Lambert PC, et al. Screening and cervical cancer cure: population based cohort study[J]. BMJ, 2012, 344: e900. doi: 10.1136/bmj.e900
-
期刊类型引用(5)
1. 安俊达,李玉双. 基于超声图像评估甲状腺和乳腺病变的通用计算方法. 燕山大学学报. 2024(01): 86-94 .  百度学术
百度学术
2. 杨茜雯,宋博,高婷婷,薛无瑕,李立坤,纪永章. 2021—2022年某三甲医院体检人群重要异常结果分布特征分析. 健康体检与管理. 2024(02): 174-177+202 .  百度学术
百度学术
3. 杨倩倩,夏源,张云飞,杨桂云,郭文佳,张秀华. 基于列线图的女性乳腺癌患者再发第二原发性甲状腺癌风险预测模型的构建和验证. 中国医药导报. 2024(24): 117-124 .  百度学术
百度学术
4. 阙厦丹,陈敦雁. 乳腺良性肿瘤和恶性肿瘤与自身免疫性甲状腺疾病的关系. 慢性病学杂志. 2023(05): 755-757 .  百度学术
百度学术
5. 王婷. 中西医结合治疗乳腺癌术后甲状腺结节的临床疗效. 世界复合医学. 2022(04): 109-111+116 .  百度学术
百度学术
其他类型引用(1)



 下载:
下载: