Relationship of Expression Difference of miR-658 and miR-492 with Pelvic Lymph Node Metastasis from Squamous Carcinoma of Cervix
-
摘要:目的
寻找宫颈鳞癌盆腔淋巴结转移相关的microRNAs。
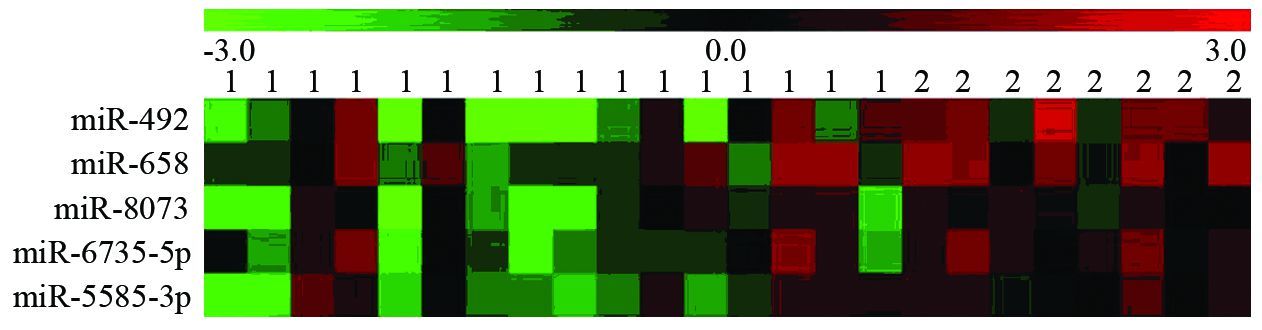
方法采用Affymetrix miRNA 4.0芯片筛查宫颈鳞癌淋巴结转移组(n=8)和未转移组患者(n=16)癌组织中差异表达的microRNAs;并选择表达差异较大的2种microRNAs,采用实时定量RT-PCR法进行验证。
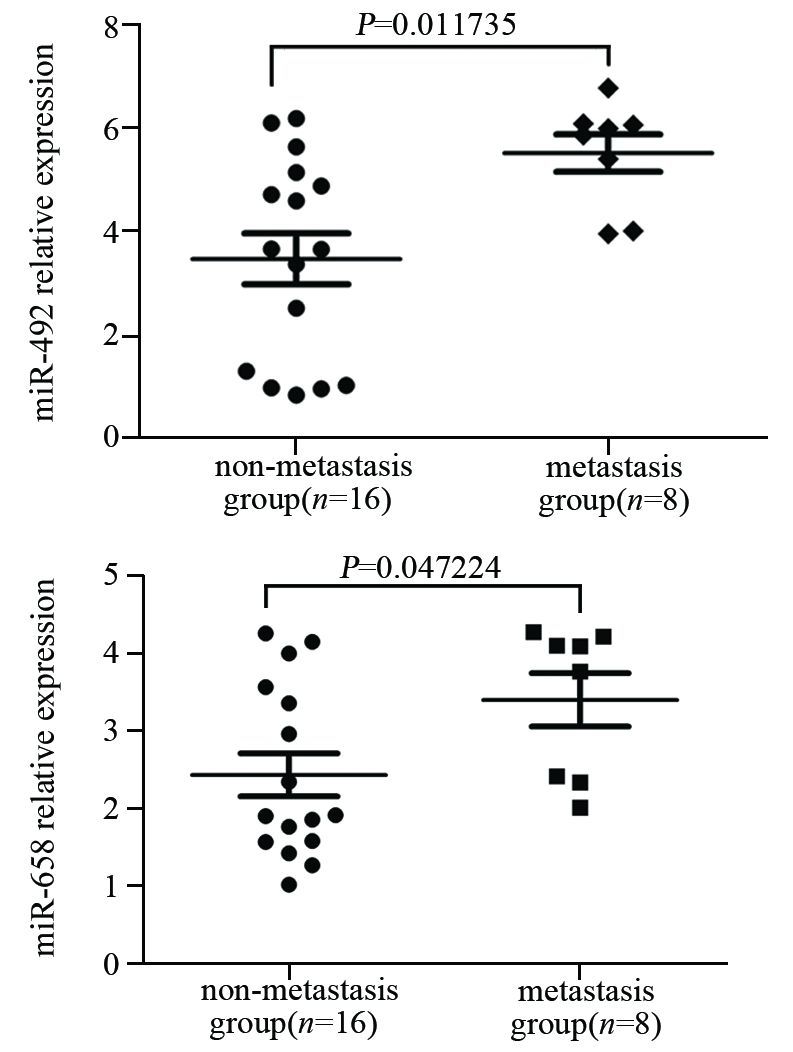
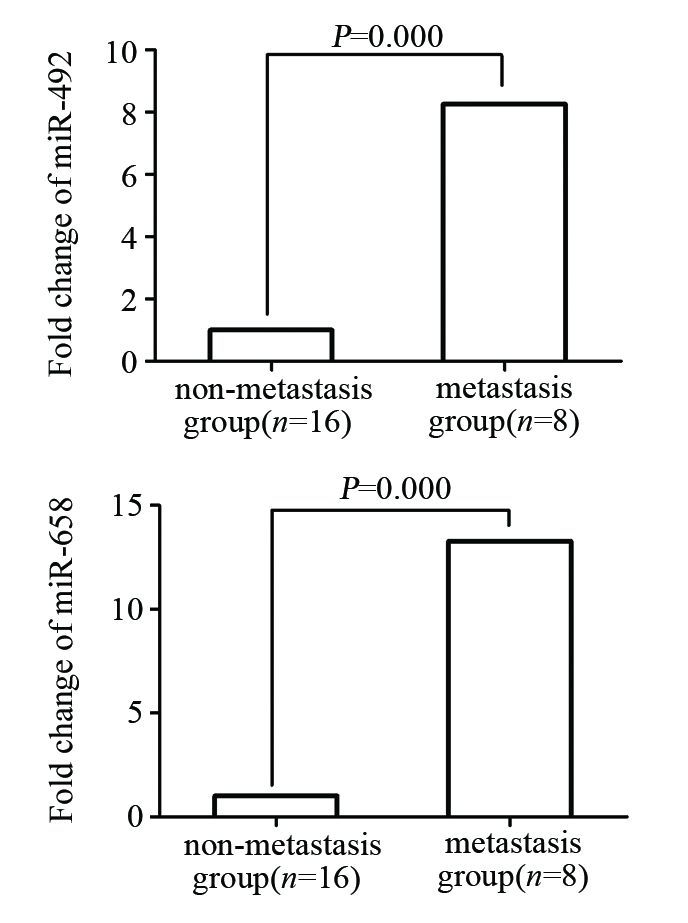
结果miRNA芯片筛查出两组间有5个microRNA存在差异表达,分别为miR-5585-3p、miR-6735-5p、miR-8073、miR-658和miR-492。且淋巴结转移组均为表达上调,其中以miR-658和miR-492的上调倍数最大,分别为4.24和5.43。实时定量RT-PCR检测miR-658和miR-492组间差异与miRNA芯片筛查
结果基本一致。
结论miR-658和miR-492表达上调可能与宫颈鳞癌盆腔淋巴结转移有关。
Abstract:ObjectiveTo explore the microRNAs which are responsible for the pelvic lymph node metastasis of squamous carcinoma of the cervix (SCC).
MethodsThe different expression of miRNAs between cancer tissue samples from SCC patients with lymph node metastasis (metastasis group, n=8) and without lymph node metastasis (non-metastasis group, n=16) were analyzed by Affymetrix miRNA 4.0 arrays. Two miRNAs which showed significant differences were validated by real-time quantification PCR.
ResultsThere were five miRNAs whose expression levels were increased in the samples from SCC patients with lymph node metastasis compared with those without lymph node metastasis, in which miR-658 and miR-492 showed significant higher folds of expression level (4.24 and 5.43) than others. The different expression of the above two miRNAs measured by real-time quantificative PCR were consistent with the result of microarrays.
ConclusionThe upregulation of miR-658 and miR-492 expression might be related with the progress of pelvic lymph node metastasis from SCC.
-
Key words:
- Squamous carcinoma of cervix /
- microRNAs /
- Lymph node metastasis /
- Microarray
-
0 引言
白血病发病率相对较小[1],但生存率较低(19.6%)[2],因此,严重影响儿童及老年人的身体健康,是造成居民巨大疾病负担的癌症之一[3-4]。昆山市位居上海与苏州之间,特殊的区位优势使得近20年经济社会快速发展,在昆山市肿瘤粗死亡率明显上升的背景下[5],本研究利用1993—2014年昆山市死因监测的白血病死亡数据,以探究其死亡率的时间趋势。
1 资料与方法
1.1 研究对象来源
江苏省昆山市于1981年全面开展全人群死因监测工作[5]。昆山市所有社区卫生服务机构及医院开展死因常规监测,同时疾控中心通过定期与公安、殡葬、妇幼保健及福利院等多部门合作,多途径收集死亡名单并开展死亡原因调查;市镇两级从业人员通过定期举办培训班、认真规范填写死亡证、逐条数据审核、现场督导检查及定期开展漏报调查等方式,来保证全市死因监测工作的质量。此外,也与苏州市范围内的其他县(市)进行数轮的数据质量互审,重点对数据的完整性、原始数据的逻辑性、统计分类及ICD-10编码以及是否重卡等进行检查、修正。昆山市所有死亡病例开具《居民死亡医学证明(推断)书》其登记报告项目包括:(1)病例人口学特征(姓名、性别、出生日期、民族、婚姻、文化程度、职业等)。(2)死亡信息:死亡原因(直接死因、间接死因、根本死因以及其他重要医学情况)、死亡日期、死亡地点等。(3)诊断信息:疾病最高诊断单位、疾病最高诊断依据等内容。(4)调查记录。年初与年末人口数来源于昆山市公安局,以计算年均观察人年数,1981—2013年年均观察人年数(年均人口数)详参文献[5]。
按照《国际疾病分类》(ICD-10)对所有恶性肿瘤疾病进行编码,白血病ICD-10编码为C91-95。根据《中国肿瘤登记工作指导手册》,并参照国际癌症研究中心(IARC)/国际癌症登记协会(IACR)对登记材料的有关要求,对肿瘤登记的完整性和可靠性进行了评估。
1.2 数据分析
采用SAS9.3统计软件进行数据分析,计算年份、性别粗死亡率与年龄标化死亡率,以及绘制时间趋势图和年龄别死亡率序列图。按照第五次全国人口普查(2000年)人口结构为标准计算年龄标化死亡率。应用年度变化百分比(annual percentage change, APC)及其95%可信区间(confidence intervals, CI)分析粗死亡率与年龄标化死亡率等时间趋势,以APC其95%CI是否包含0为统计学检验标准,同时给出回归系数检验的P值[6]。
2 结果
2.1 江苏省昆山市1993—2014年白血病死亡趋势分析
江苏省昆山市1993—2014年期间白血病死亡总例数为570例(男312例,女258例),占全肿瘤比例为2.19%;总的来看昆山市1993—2014年白血病死亡数明显上升(APC=3.0, 95%CI: 1.6~4.4, P=0.0007)。
江苏省昆山市白血病粗死亡率由1993年的4.01/10万上升到2014年的4.99/10万,上升趋势没有统计学意义(APC=1.5, 95%CI: 0.0~3.0, P=0.0604)。在男性人群中白血病粗死亡率由1993年的4.53/10万上升到2014年的5.02/10万,上升趋势无明显统计学意义(APC=0.8, 95%CI: -0.6~2.2, P=0.2756);女性人群中白血病粗死亡率由1993年的3.49/10万上升到2014年的4.96/10万,上升趋势无统计学意义(APC=2.7, 95%CI: 0.0~5.4, P=0.0622)。1993—2014年白血病中标死亡率在男女合计人群中无明显变化趋势(APC=1.5, 95%CI: 0.0~3.0, P=0.0604);男性(APC=-0.7, 95%CI: -2.4~1.0, P=0.4087)和女性(APC=0.4, 95%CI: -2.3~3.1, P=0.7612)人群中白血病中标死亡率没有明显变化趋势,见图 1、表 1。
1993—2014年白血病死亡率其0~74岁累积死亡率由1993年的0.33%上升到2014年的0.38%(APC=0.7, 95%CI: -0.9~2.3, P=0.4168),没有发现白血病死亡的风险在0~74岁年龄组随着时间有明显变化,见表 1。
表 1 江苏省昆山市1993—2014年白血病死亡率分析Table 1 Mortality of leukemia in Kunshan City, Jiangsu Province, 1993-2014
2.2 江苏省昆山市1993—2014年白血病年龄别死亡率分析
1993—2004年,白血病年龄别死亡率在60之前处于低水平,60岁以后缓慢上升,至65~69岁达到高峰,70岁以后白血病死亡率明显下降。2005—2014年,白血病年龄别死亡率在60之前处于低水平,60岁以后开始明显抬升,至70~74岁达到高峰,75岁以后白血病死亡率略有下降。与1993—2004年相比,2005—2014年白血病年龄别死亡率明显偏高,特别是60岁以上年龄段,见图 2、表 2。
表 2 江苏省昆山市白血病年龄别死亡率分析Table 2 Age-specific mortality of leukemia by gender in Kunshan City, Jiangsu Province
3 讨论
在江苏省昆山市肿瘤中标死亡率总体呈现下降趋势的情况下[5],人口老龄化与其他危险因素一起促进了肿瘤死亡的变化。在昆山市肿瘤死亡率明显上升的肺癌中这种促进因素最为明显[7]。虽然昆山市白血病占全肿瘤死亡(2.19%)的比例较低;但是由于发病年龄较早、生存率较低及预后差[2],造成的疾病负担较大。
昆山市白血病死亡率位居肿瘤死亡顺位第9位[8-9]。同期与全国白血病死亡率相比,昆山地区死亡率明显低于全国2009年水平(世标率,2.66/10万 vs. 3.35/10万)[10],也低于全国2012年水平(2.48/10万 vs. 3.13/10万)[11]。就死亡率趋势来看,昆山市1993—2014年白血病中标死亡率趋势则没有明显的变化(APC=1.5, 95%CI: 0.0~3.0, P=0.0604)。浙江省2000—2009年白血病死亡率明显上升(APC=5.09, 95%CI: 1.13~9.21)[12],此外还有山东省(1970—2005年)[13]。除了单独看白血病死亡率,白血病发病率的高低不容忽视。与昆山市相邻的浙江省2000—2009年白血病的发病率明显上升(APC=3.21, 95%CI: 0.20~6.30)[12],此外上海[14]与南京地区[4]白血病发病率也明显上升。
从白血病年龄别死亡率来看,本研究显示白血病年龄别死亡率呈现明显的两个高峰,即20岁以下年龄组与65岁以上年龄组,与上海和浙江等地区的研究结果基本一致[4, 12, 14];也与全国肿瘤登记的结果一致[15]。年龄别死亡率的差异提示白血病的发病可能是暴露因素的差异所致。白血病的发生是基因与环境共同作用的结果。经济社会状态也是影响白血病发生的因素[16]。环境因素中饮食模式是影响白血病发生的因素之一[17-18];父母早期的不良生活方式暴露是影响儿童白血病的因素,如烟草、酒精等[19-20]。
虽然江苏省昆山市1993—2014年白血病死亡率趋势变化不明显;但是随着户籍人口逐年增加,因白血病而死亡的例数明显上升,疾病负担加大。在继续强化监测工作以观察其时间趋势的同时,也要考虑进一步加强监测工作质量控制。江苏省昆山市于1981年全面开展死因监测[5];在2013年加入国家疾病监测点,在加入监测点之前于2011—2012年开展了死亡漏报调查,结果显示漏报率为0.34%,提示既往的死因监测处于可接受区间[21]。
-
表 1 24例宫颈鳞癌患者的临床和病理资料
Table 1 Clinicopathological data of 24 patients with squamous carcinoma of cervix (SCC)

表 2 miRNA芯片检测到的淋巴结转移组与未转移组间存在表达差异的5个miRNAs
Table 2 Five differentially-expressed miRNAs between metastasis group and non-metastasis group detected by microarrays

-
[1] Jemal A, Bray F, Center MM, et al. Global cancer statistics[J]. CA Cancer J Clin, 2011, 61(2): 69-90. [1] Jemal A, Bray F, Center MM, et al. Global cancer statistics[J]. CA Cancer J Clin, 2011, 61(2): 69-90. doi: 10.3322/caac.v61:2
[2] 胡尚英, 郑荣寿, 赵方辉, 等. 1989至2008年中国女性子宫颈癌发病和死亡趋势分析[J]. 中国医学科学院学报, 2014, 36(2): 119-25. http://www.cnki.com.cn/Article/CJFDTOTAL-ZYKX201402001.htm Hu SY, Zheng RS, Zhao FH, et al. Trend analysis of cervical cancer incidence and mortality rates in chinese women during 1989-2008[J]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao, 2014, 36(2): 119-25. http://www.cnki.com.cn/Article/CJFDTOTAL-ZYKX201402001.htm
[2] 胡尚英, 郑荣寿, 赵方辉, 等. 1989至2008年中国女性子宫颈癌 发病和死亡趋势分析[J]. 中国医学科学院学报, 2014, 36(2): 11 9-25. [Hu SY, Zheng RS, Zhao FH, et al. Trend analysis of cervical cancer incidence and mortality rates in chinese women during 1989-2008[J]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao, 20 14, 36(2): 119-25.] [3] Alvarez RD, Soong SJ, Kinney WK, et al. Identification of prognostic factors and risk groups in patients found to have nodal metastasis at the time of radical hysterectomy for early-stage squamous carcinoma of the cervix[J]. Gynecol Oncol, 1989, 35 (2):130-5. [3] Alvarez RD, Soong SJ, Kinney WK, et al. Identification of prognostic factors and risk groups in patients found to have nodal metastasis at the time of radical hysterectomy for early-stage squamous carcinoma of the cervix[J]. Gynecol Oncol, 1989, 35(2):130-5. doi: 10.1016/0090-8258(89)90029-2
[4] Liu MT, Hsu JL, Liu WS, et al. Prognostic factors affecting the outcome of early cervical cancer treated with radical hysterectomy and post-operative adjuvant therapy[J]. Eur J Cancer Care(Engl), 2008, 17(2): 174-81. doi: 10.1111/ecc.2008.17.issue-2
[4] Liu MT, Hsu JL, Liu WS, et al. Prognostic factors affecting the outcome of early cervical cancer treated with radical hysterectomy and post-operative adjuvant therapy[J]. Eur J Cancer Care(Engl), 20 08, 17(2): 174-81. [5] Dietrich D, Krispin M, Dietrich J, et al. CDO1 promoter methylation is a biomarker for outcome prediction of anthracycline treated, estrogen receptor-positive, lymph nodepositive breast cancer patients[J]. BMC Cancer, 2010, 10: 247. [5] Dietrich D, Krispin M, Dietrich J, et al. CDO1 promoter methylation is a biomarker for outcome prediction of anthracycline treated, estrogen receptor-positive, lymph node-positive breast cancer patients[J]. BMC Cancer, 2010, 10: 247. doi: 10.1186/1471-2407-10-247
[6] Salhia B, Kiefer J, Ross JT, et al. Integrated genomic andepigenomic analysis of breast cancer brain metastasis[J]. PLoS One, 2014, 9(1): e85448. [6] Salhia B, Kiefer J, Ross JT, et al. Integrated genomic and epigenomic analysis of breast cancer brain metastasis[J]. PLoS One, 2014, 9(1): e85448. doi: 10.1371/journal.pone.0085448
[7] Granados López AJ, López JA. Multistep model of cervical cancer: participation of miRNAs and coding genes[J]. Int J Mol Sci, 2014, 15(9): 15700-33. doi: 10.3390/ijms150915700
[7] Granados López AJ, López JA. Multistep model of cervical canc er: participation of miRNAs and coding genes[J]. Int J Mol Sci, 20 14, 15(9): 15700-33. [8] Zhang BG, Li JF, Yu BQ, et al. microRNA-21 promotes tumor proliferation and invasion in gastric cancer by targeting PTEN[J]. Oncol Rep, 2012, 27(4): 1019-26. http://cn.bing.com/academic/profile?id=2023036676&encoded=0&v=paper_preview&mkt=zh-cn
[8] Zhang BG, Li JF, Yu BQ, et al. microRNA-21 promotes tumor proliferation and invasion in gastric cancer by targeting PTEN[J]. Oncol Rep, 2012, 27(4): 1019-26. [9] Lin CW, Chang YL, Chang YC, et al. MicroRNA-135b promotes lung cancer metastasis by regulating multiple targets in the Hippo pathway and LZTS1[J]. Nat Commun, 2013, 4: 1877. doi: 10.1038/ncomms2876
[9] Lin CW, Chang YL, Chang YC, et al. MicroRNA-135b promotes lung cancer metastasis by regulating multiple targets in the Hippo pathway and LZTS1[J]. Nat Commun, 2013, 4: 1877. [10] Zhao Y, Deng C, Wang J, et al. Let-7 family miRNAs regulate estrogen receptor alpha signaling in estrogen receptor positive breast cancer[J]. Breast Cancer Res Treat, 2011,127(1): 69-80. [10] Zhao Y, Deng C, Wang J, et al. Let-7 family miRNAs regulate estrogen receptor alpha signaling in estrogen receptor positive breast cancer[J]. Breast Cancer Res Treat, 2011,127(1): 69-80. doi: 10.1007/s10549-010-0972-2
[11] Garzon R, Calin GA, Croce CM. MicroRNAs in cancer[J]. Annu Rev Med, 2009, 60: 167-79. [11] Garzon R, Calin GA, Croce CM. MicroRNAs in cancer[J]. Annu Rev Med, 2009, 60: 167-79. doi: 10.1146/annurev.med.59.053006.104707
[12] Albulescu R, Neagu M, Albulescu L, et al. Tissular and soluble miRNAs for diagnostic and therapy improvement in digestive tract cancers[J]. Expert Rev Mol Diagn, 2011, 11(1): 101-20. [12] Albulescu R, Neagu M, Albulescu L, et al. Tissular and soluble miRNAs for diagnostic and therapy improvement in digestive tract cancers[J]. Expert Rev Mol Diagn, 2011, 11(1): 101-20. doi: 10.1586/erm.10.106
[13] Roa W, Brunet B, Guo L, et al. Identification of a new microRNA expression profile as a potential cancer screening tool[J]. Clin Invest Med, 2010, 33(2): E124. [13] Roa W, Brunet B, Guo L, et al. Identification of a new microRNA expression profile as a potential cancer screening tool[J]. Clin Invest Med, 2010, 33(2): E124. http://cn.bing.com/academic/profile?id=1522716087&encoded=0&v=paper_preview&mkt=zh-cn
[14] Calin GA, Liu CG, Sevignani C, et al. MicroRNA profiling reveals distinct signatures in B cell chronic lymphocytic leukemias[J].Proc Natl Acad Sci U S A, 2004, 101(32): 11755-60. doi: 10.1073/pnas.0404432101
[14] Calin GA, Liu CG, Sevignani C, et al. MicroRNA profiling reveals distinct signatures in B cell chronic lymphocytic leukemias[J]. Proc Natl Acad Sci U S A, 2004, 101(32): 11755-60. [15] Yao T, Lin Z. MiR-21 is involved in cervical squamous cell tumorigenesis and regulates CCL20[J]. Biochim Biophys Acta, 20 12, 1822(2): 248-60. [15] Yao T, Lin Z. MiR-21 is involved in cervical squamous cell tumorigenesis and regulates CCL20[J]. Biochim Biophys Acta, 2012, 1822(2): 248-60. doi: 10.1016/j.bbadis.2011.09.018
[16] 曾康康, 莫祥兰, 刘斐, 等. 宫颈癌及癌前病变组织中microRNAs 的差异表达[J]. 肿瘤防治研究, 2014, 41(7): 789-93. [Zeng KK, Mo XL, Liu F, et al. Differential expression of microRNAs in cervical cancer and cervical precancerous lesions[J]. Zhong Liu Fang Zhi Yan Jiu, 2014, 41(7): 789-93.] [16] 曾康康, 莫祥兰, 刘斐, 等. 宫颈癌及癌前病变组织中microRNAs的差异表达[J]. 肿瘤防治研究, 2014, 41(7): 789-93. http://www.zlfzyj.com/CN/article/searchArticle.do# Zeng KK, Mo XL, Liu F, et al. Differential expression of microRNAs in cervical cancer and cervical precancerous lesions[J]. Zhong Liu Fang Zhi Yan Jiu, 2014, 41(7): 789-93. http://www.zlfzyj.com/CN/article/searchArticle.do#
[17] von Frowein J, Pagel P, Kappler R, et al. MicroRNA-492 is processed from the keratin 19 gene and up-regulated in metastatic hepatoblastoma[J]. Hepatology, 2011, 53(3): 833-42. doi: 10.1002/hep.24125
[17] von Frowein J, Pagel P, Kappler R, et al. MicroRNA- 4 9 2 i s p r o c e s s e d f r om t h e k e r a t i n 19 g e n e a n d u p - regulated in metastatic hepatoblastoma[J]. Hepatology, 2011, 53 (3): 833-42. [18] Gaedcke J, Grade M, Camps J, et al. The rectal cancer microRNAome-microRNA expression in rectal cancer and matched normal mucosa[J]. Clin Cancer Res, 2012, 18(18): 4919-30. doi: 10.1158/1078-0432.CCR-12-0016
[18] Gaedcke J, Grade M, Camps J, et al. The rectal cancer microRNAome-microRNA expression in rectal cancer and matched normal mucosa[J]. Clin Cancer Res, 2012, 18(18): 49 19-30. [19] Schultz NA, Werner J, Willenbrock H, et al. MicroRNA expression profiles associated with pancreatic adenocarcinoma and ampullary adenocarcinoma[J]. Mod Pathol, 2012, 25(12): 1609-22. doi: 10.1038/modpathol.2012.122
[19] Schultz NA, Werner J, Willenbrock H, et al. MicroRNA expression profiles associated with pancreatic adenocarcinoma and ampullary adenocarcinoma[J]. Mod Pathol, 2012, 25(12): 1609-22. [20] Jiang J, Zhang Y, Yu C, et al. MicroRNA-492 expression promotes the progression of hepatic cancer by targeting PTEN[J]. Cancer Cell Int, 2014, 14(1): 95. [20] Jiang J, Zhang Y, Yu C, et al. MicroRNA-492 expression promotes the progression of hepatic cancer by targeting PTEN[J]. Cancer Cell Int, 2014, 14(1): 95. doi: 10.1186/s12935-014-0095-7
[21] Shen F, Cai WS, Feng Z, et al. MiR-492 contributes to cell proliferation and cell cycle of human breast cancer cells by suppressing SOX7 expression[J]. Tumour Biol, 2015, 36(3): 19 13-21. [21] Shen F, Cai WS, Feng Z, et al. MiR-492 contributes to cell proliferation and cell cycle of human breast cancer cells by suppressing SOX7 expression[J]. Tumour Biol, 2015, 36(3): 1913-21. doi: 10.1007/s13277-014-2794-z
[22] Cummins JM, He Y, Leary RJ, et al. The colorectal microRNA-ome[J]. Proc Natl Acad Sci U S A, 2006, 103(10): 3687-92. doi: 10.1073/pnas.0511155103
[22] Cummins JM, He Y, Leary RJ, et al. The colorectal microRNAome[ J] Proc Natl Acad Sci U S A, 2006, 103(10): 3687-92. [23] Guo J, Miao Y, Xiao B, et al. Differential expression of microRNA species in human gastric cancer versus non-tumorous tissues[J]. J Gastroenterol Hepatol, 2009, 24(4): 652-7. doi: 10.1111/jgh.2009.24.issue-4
[23] Guo J, Miao Y, Xiao B, et al. Differential expression of microRNA species in human gastric cancer versus non-tumorous tissues[J]. J Gastroenterol Hepatol, 2009, 24(4): 652-7.




 下载:
下载: