Effect of Operation Incision Selection on Success rate of Sentinel Lymph Node Biopsy and Subcutaneous Hydrops in Breast Cancer
-
摘要:目的
探讨不同手术切口对乳腺癌行前哨淋巴结活检成功率及皮下积液发生情况的影响。
方法回顾分析2011—2013年南昌市第三医院乳腺一科收治的乳腺癌病例,依条件排除后共132例入组。69例行乳房加腋窝横行双切口手术,63例行乳房延伸至腋窝单切口手术。比较两种手术切口方式下前哨淋巴结的检出率、患者切口引流时间以及皮下积液发生率的差异。
结果单切口组与双切口组,前哨淋巴结检出率分别为96.8%与97.1%,差异无统计学意义(P>0.05)。当前哨淋巴结为阴性时,双切口组与单切口组患者术后切口引流时间比较,差异无统计学意义(P>0.05);当前哨淋巴结为阳性时,双切口组与单切口组患者术后切口引流时间比较,差异有统计学意义(P<0.05);当前哨淋巴结为阴性时,双切口组患者腋下积液发生率为23.8%,单切口组为7.5%,差异有统计学意义(P<0.05);当前哨淋巴结为阳性时,双切口组患者腋下积液发生率为28.0%,单切口组为23.8%,两组比较差异有统计学意义(P<0.05)。
结论术前腋窝淋巴结评估为阴性的患者选择单切口将更有利于降低患者术后皮下积液的发生率且引流时间短于双切口组,而术前腋窝淋巴结评估为阳性的患者两种手术切口方式在术后皮下积液的发生率以及带管时间上未见差异。
Abstract:ObjectiveTo investigate the effect of operation incision selection on the success rate of sentinel lymph node biopsy and subcutaneous hydrops in breast cancer.
MethodsA retrospective analysis of 132 cases of breast cancer were enrolled from the Third Hospital of Nanchang from 2011 to 2013. Sixty-nine cases received breast plus axillary incision surgery, and 63 cases received breast extended to axillary incision surgery. The detection rate of sentinel lymph nodes, incision drainage time and the incidence of subcutaneous effusion were compared between both groups.
ResultsThe successful rate of sentinel lymph node detection in single incision group and double incision group were 96.8% and 97.1%, respectively(P>0.05). When the sentinel lymph nodes were negative, the difference of drainage time between two groups had no statistical significance (P>0.05), the incidence of axillary hydrops of double incision group and single incision group were 23.8% and 7.5% (P<0.05); while when the sentinel lymph nodes were positive, the difference of drainage time between two groups had statistical significance (P<0.05). The incidence of axillary hydrops between two groups were 28.0% and 23.8% (P<0.05).
ConclusionPreoperative axillary lymph node assessment is helpful for negative patients to select single incision, which is beneficial to reduce the incidence of postoperative subcutaneous effusion and drainage time in comparison with double incision group. As for positive patients, preoperative axillary lymph node assessment has no effect on the incidence of postoperative subcutaneous effusion or the time of tube between two types of surgical incision.
-
Key words:
- Operation incision /
- Breast cancer /
- Sentinel lymph node biopsy /
- Subcutaneous hydrops
-
0 引言
早期乳腺癌行腋窝前哨淋巴结活检(sentinel lymph node biopsy, SLNB)已迅速替代腋窝淋巴结清除术(axillary lymph node dissection, ALND)成为早期乳腺癌的标准治疗。作为一项腋窝准确分期的微创活检技术,SLNB代表着乳腺癌外科治疗的发展水平。大样本前瞻性随机试验结果包括英国ALMANAC试验(1)[1]、意大利米兰SNB185试验(2)[2]和美国NSABPB-32试验(3)[3]均证实SLNB可以提供准确的腋窝淋巴结分期,是能准确评估腋窝淋巴结[4]的一种方法,现在腋窝前哨淋巴结活检大多选择乳房切口加腋窝切口,该方法有一些患者腋窝处出现了积液及瘢痕组织的形成,影响了患侧上肢的活动。本研究旨在探讨乳房加腋窝横行双切口与乳房向下方延伸至腋窝单切口这两种切口方式的选择对腋窝前哨淋巴结检出率、患者术后带管时间及皮下积液的影响。
1 资料与方法
1.1 一般资料
回顾性分析2011—2013年南昌市第三医院乳腺肿瘤科收治的乳腺癌患者的病历资料,其中男性患者2例,有乳腺恶性肿瘤家族史的患者5例,女性患者中有42例已绝经,中位年龄46岁,排除既往已行腋窝手术史以及分期为Ⅲ、Ⅳ期的患者共132例入组。所有患者均于术前行空心针穿刺活检病理确诊为浸润性乳腺癌。其中69例选择了乳房加腋窝横行双切口,63例选择了乳房向下方延伸至腋窝单切口。
1.2 方法
术前15 min将亚甲蓝2~4 ml(美蓝,质量分数1%,北京永康制药厂)皮下注射于乳头乳晕下皮下组织内,注射区域按摩2~3 min。
1.2.1 双切口组
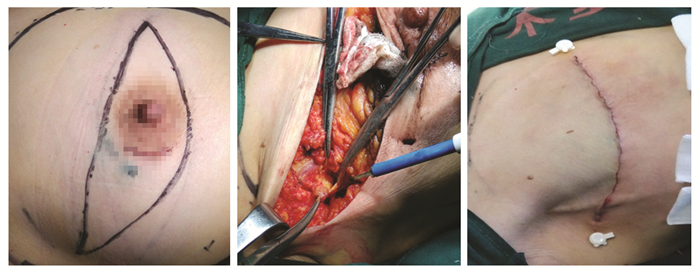
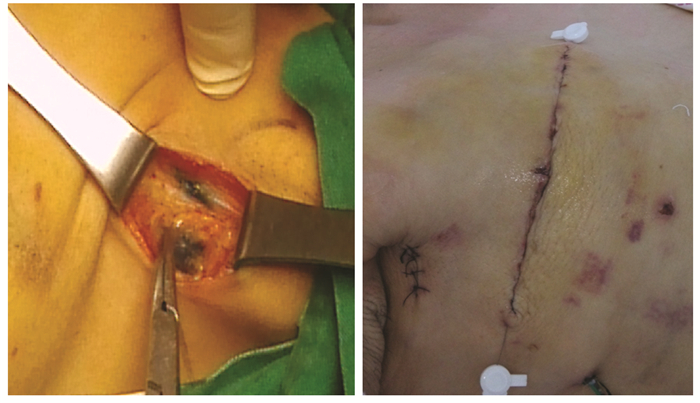
双切口组注射15 min后在腋窝顶部下方3横指位置取3 cm左右手术切口,切开皮肤及皮下组织,脂肪层可见蓝染淋巴管。在胸大肌外侧附近逐一摘除蓝染淋巴结,送检。如前哨淋巴结阴性,手术创面放置皮片引流,再行同侧乳房单纯切除。第二天拔出皮片。如前哨淋巴结阳性,则行乳房单纯切除并延长腋窝切口行腋窝清扫术,见图 1。
1.2.2 单切口组
单切口组注射15 min后自原发肿瘤外缘向腋窝分离脂肪、结缔组织,发现蓝染的淋巴管后,向乳腺尾部寻找距离体中心最近的蓝染淋巴结,将该淋巴结切除,送检。如前哨淋巴结阴性,乳房切除术后放置引流管引流。如前哨淋巴结阳性,原切口行腋窝清扫术后放置引流管引流,见图 2。
1.2.3 查阅病例资料比较两组前哨淋巴结的检出率、术后引流时间以及皮下积液的发生率
有关皮下积液的定义采用Dalberg皮下积液诊断标准[5],即术后第5天引流量仍>30 ml或引流管拔除后第2天术区皮下有波动感,且穿刺皮下抽出液体量>5 ml。
1.3 统计学方法
采用SPSS10.0统计软件进行数据分析。应用χ2检验和两独立样本t检验比较不同手术切口的选择对腋窝前哨淋巴结活检检出率以及术后患者皮下积液情况差异的影响。P<0.05为差异有统计学意义。
2 结果
2.1 不同手术切口的选择对腋窝前哨淋巴结活检成功率的影响
69例双切口组中67例检出前哨淋巴结(SLN) (其中前哨阴性42例、前哨阳性25例),检出率为97.1%。检出SLN 1枚者19例、2枚者30例、3枚者12例、4枚者4例、5枚者2例。63例单切口组中61例检出SLN(其中前哨阴性40例、前哨阳性21例),检出率为96.8%。检出SLN 1枚者18例、2枚者28例、3枚者13例、4枚者2例、5枚者0例。两组SLN检出率差异无统计学意义(χ2=0.009, P=0.926)。
2.2 不同手术切口的选择对术后引流时间的影响
前哨淋巴结阴性时,双切口组平均引流时间为(8.90±2.469)天,而单切口组平均引流时间为(7.46±2.146)天,两组比较差异有统计学意义(t=9.432, P<0.001)。前哨淋巴结阳性行腋窝清扫术后,双切口组平均引流时间为(13.60±3.177)天,单切口组平均引流时间为(12.80±2.386)天,两组比较差异无统计学意义(t=1.586,P=0.115)。
2.3 皮下积液发生率
当前哨淋巴结阴性时,双切口组第二天拔出皮片后42例SLN阴性中有10例发生腋下积液,发生率为23.8%。单切口组拔出引流管后40例SLN阴性中仅有3例发生皮下积液,发生率为7.5%。两组比较差异有统计学意义(χ2=4.085, P=0.043)。当前哨淋巴结阳性行腋窝清扫术后,双切口组SLN阳性25例中有7例发生皮下积液,发生率为28.0%。单切口组21例SLN阳性中有5例发生皮下积液,发生率为23.8%。两组比较差异无统计学意义(χ2=0.104, P=0.747)。
3 讨论
乳腺癌是女性最常见的恶性肿瘤之一,其发病率占全身恶性肿瘤的7%~10%[5]。我国乳腺癌发病率正以3%的速度迅速增长[6-7]。近年来,早期乳腺癌行前哨淋巴结活检(SLNB)是继保乳手术后最重要的进展之一。一般认为,若SLN无转移,原发肿瘤引流区域中的其他淋巴结也不会发生恶性肿瘤细胞的转移,如果SLN阳性,则区域淋巴结有可能受累,那么其病理学诊断可代表整个区域淋巴结的病理学状态[8-9]。
目前,腋窝前哨淋巴结活检大多选择乳房切口加腋窝切口,有部分患者会出现腋窝处积液及瘢痕组织的形成,影响其患侧上肢的活动。为此,我们将此法与单乳房切口延伸向腋窝下方的方法进行比较,分析手术切口的选择对腋窝前哨淋巴结活检、术后康复及皮下积液的影响。从解剖学角度讲,SLN是收纳某器官某区域组织淋巴液的第一站淋巴结[10],具体到乳腺,即为乳腺癌癌细胞转移的第一站淋巴结。乳腺癌SLN示踪定位方法是以乳房和局部区域淋巴系统的功能和解剖特点为组织学基础[11],在乳房肿块周围注入染料或特定的物质,可以随着淋巴回流至区域淋巴结。Creager等[12]用联合法对75例多中心病灶的乳腺癌患者进行SLNB,示踪剂注射于肿瘤区域皮下组织,SLNB后常规行ALND。71例成功检测出SLN,检出率为94.7%,3例SLN阴性者ALND后病理证实非SLN阳性,假阴性率为8.8%。研究认为,示踪剂的不同注射部位不影响SLNB的准确性,对SLN解剖定位无影响。本课题主要通过注射于乳头乳晕下部位比较单双切口的不同,结果显示两种方法均能够清楚的显示淋巴管及淋巴结,发现两种切口对前哨淋巴结检出率的差异无统计学意义(χ2=0.009, P=0.926),同时分析得知如果术前腋窝评估可能为阴性患者,选择单切口可以获得更低的皮下积液发生率,和双切口比较,差异具有统计学意义(χ2=4.085, P=0.043),并且患者的带管时间更短(t=9.432, P<0.001),而对于术前评估腋窝淋巴结阳性患者,以上两种手术切口方式的选择对患者术后皮下积液发生率(χ2=0.104, P=0.747)以及引流时间(t=1.586, P=0.115)的差异无统计学意义。
同时,本课题中我们也分析了一般乳腺癌术后皮下积液的原因:(1)引流不畅使创面的渗出液不能及时引出而积聚[11];(2)创面内血液凝固形成凝血块,不能引流出以后液化形成积液[13];(3)解剖腋静脉周围的淋巴脂肪时,一些小的淋巴管损伤而未结扎,伴引流不畅形成积液,一般发生在腋窝外侧;(4)用电刀解剖腋静脉时,发生积液的机会较使用手术刀为多,可能电刀对创面的愈合有一定的影响,且经电刀解剖后一些小的淋巴管暂时封闭,而在负压吸引后又有开放造成积液[14];(5)此外皮瓣张力过大使伤口不易覆盖以及引流管拔除过早等也有一定的关系。
因此,本研究认为前腋窝评估显示为阴性患者应选择单切口,无论在引流时间及皮下积液发生率上均优于双切口,如果腋窝淋巴结评估为阳性,则单双切口的选择将没有差异。
-
-
[1] Soteldo J, Ratto EL, Gandini S, et al. Pelvic sentinel lymph node biopsy in melanoma patients: is it worthwhile?[J]. Melanoma Res, 2010, 20(2): 133-7. doi: 10.1097/CMR.0b013e3283324e40
[1] Soteldo J, Ratto EL, Gandini S, et al. Pelvic sentinel lymph node biopsy in melanoma patients: is it worthwhile?[J]. Melanoma Res, 20 10, 20(2): 133-7. [2] Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-noderesection compared with conventional axillary 1ymph-nodedissection in clinically node-negative patients with breast cancer: overall smvival findings from the NSABP B-32 randomised phase3 trial[J]. Lancet Oncol, 2010, 11(2): 927-33.
[2] Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymphnoderesection compared with conventional axillary 1ymphnodedissection in clinically node-negative patients with breast cancer: overall smvival findings from the NSABP B-32 randomised phase3 trial[J]. Lancet Oncol, 2010, 11(2): 927-33. [3] Aoyama K, Kamio T, Ohchi T, et al. Sentinel lymph node biopsy for breast eancer patients using fluorescence navigation with indocyanine green[J]. World J Surg Oncol, 2011, 9: 157. [3] Aoyama K, Kamio T, Ohchi T, et al. Sentinel lymph node biopsy for breast eancer patients using fluorescence navigation with indocyanine green[J]. World J Surg Oncol, 2011, 9: 157. doi: 10.1186/1477-7819-9-157
[4] Yang R,Wang SJ, Zhang Y, et al. Progress and prospect of methylene blue as lymph tracer[J]. Zhongguo Yao Ji Xue Za Zhi, 20 09, 7(2): 65-71. [杨瑞, 王淑君, 张颖, 等. 亚甲蓝作为淋巴示 踪剂的研究与展望[J]. 中国药剂学杂志, 2009, 7(2): 65-71.] [4] 杨瑞, 王淑君, 张颖, 等. 亚甲蓝作为淋巴示踪剂的研究与展望[J]. 中国药剂学杂志, 2009, 7(2): 65-71. http://www.cnki.com.cn/Article/CJFDTOTAL-PZGY200902006.htm Yang R,Wang SJ, Zhang Y, et al. Progress and prospect of methylene blue as lymph tracer[J]. Zhongguo Yao Ji Xue Za Zhi, 2009, 7(2): 65-71. http://www.cnki.com.cn/Article/CJFDTOTAL-PZGY200902006.htm
[5] Howell A, Anderson AS, Clarke RB, et al. Risk determination and prevention of breast cancer[J]. Breast Cancer Res, 2014, 16(5): 446. [5] Howell A, Anderson AS, Clarke RB, et al. Risk determination and prevention of breast cancer[J]. Breast Cancer Res, 2014, 16(5): 446. doi: 10.1186/s13058-014-0446-2
[6] Ni XJ, Zhang XL, Ou-Yang QW, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy[J]. PLoS One, 2014, 9(11): e111886. doi: 10.1371/journal.pone.0111886
[6] Ni XJ, Zhang XL, Ou-Yang QW, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy[J]. PLoS One, 2014, 9(11): e111886. [7] Yang J, Li HJ, Yang XQ, et al. Relationship of prediction of breast cancer infiltrating lymphocytes responsing to neoadjuvant chemotherapy and prognosis[J]. Huaxi Yi Xue, 2015, 30(6): 1179-82. [杨菁, 李宏江, 羊晓勤, 等. 乳腺癌浸润淋巴细胞对新辅助化学疗 法反应的预测及与预后的关系[J]. 华西医学, 2015, 30(6): 1179-82.] [7] 杨菁, 李宏江, 羊晓勤, 等. 乳腺癌浸润淋巴细胞对新辅助化学疗法反应的预测及与预后的关系[J]. 华西医学, 2015, 30(6): 1179-82. http://www.cnki.com.cn/Article/CJFDTOTAL-HXYX201506055.htm Yang J, Li HJ, Yang XQ, et al. Relationship of prediction of breast cancer infiltrating lymphocytes responsing to neoadjuvant chemotherapy and prognosis[J]. Huaxi Yi Xue, 2015, 30(6): 1179-82. http://www.cnki.com.cn/Article/CJFDTOTAL-HXYX201506055.htm
[8] Pettersson A, Graff RE, Ursin G, et al. Mammographic density phenotypes and risk of breast cancer: a meta-analysis[J]. J Natl Cancer Inst, 2014, 106(5): pii: dju078. [8] Pettersson A, Graff RE, Ursin G, et al. Mammographic density phenotypes and risk of breast cancer: a meta-analysis[J]. J Natl Cancer Inst, 2014, 106(5): pii: dju078. doi: 10.1093/jnci/dju078
[9] Haddad TC, Goetz MP. Landscape of neoadjuvant therapy for breast cancer[J]. Ann Surg Oncol, 2015, 22(5): 1408-15. doi: 10.1245/s10434-015-4405-7
[9] Haddad TC, Goetz MP. Landscape of neoadjuvant therapy for breast cancer[J]. Ann Surg Oncol, 2015, 22(5): 1408-15. [10] Chen X, Wang S. Current status andadvancer of sentinel lymph node biopsy in breast cancer[J]. Zhongguo Pu Wai Ji Chu Yu Lin Chuang Za Zhi, 2011,18(1): 98-102. [陈翔, 王水. 乳腺癌前哨淋巴结活检研 究现状及进展[J]. 中国普外基础与临床杂志, 2011, 18(1): 98-102.] [10] 陈翔, 王水. 乳腺癌前哨淋巴结活检研究现状及进展[J]. 中国普外基础与临床杂志, 2011, 18(1): 98-102. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201101038.htm Chen X, Wang S. Current status andadvancer of sentinel lymph node biopsy in breast cancer[J]. Zhongguo Pu Wai Ji Chu Yu Lin Chuang Za Zhi, 2011,18(1): 98-102. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201101038.htm
[11] Wang S, Fan P, Wu ZY. Preliminary study on lymphocyte subests of sentinel lymph nodes in breast cancer patients[J]. Zhonghua Zhong Liu Za Zhi, 2010, 26(4): 220-2. [王水, 范萍, 武正炎. 乳腺癌前哨淋巴 结淋巴细胞亚群的初步研究[J]. 中华肿瘤杂志, 2010, 26(4): 220-2.] [11] 王水, 范萍, 武正炎. 乳腺癌前哨淋巴结淋巴细胞亚群的初步研究[J]. 中华肿瘤杂志, 2010, 26(4): 220-2. http://www.cnki.com.cn/Article/CJFDTOTAL-ZHZL200404009.htm Wang S, Fan P, Wu ZY. Preliminary study on lymphocyte subests of sentinel lymph nodes in breast cancer patients[J]. Zhonghua Zhong Liu Za Zhi, 2010, 26(4): 220-2. http://www.cnki.com.cn/Article/CJFDTOTAL-ZHZL200404009.htm
[12] Creager AJ, Geisinger KR. Int raoperative evaluation of sentinel lymph nodes for breast carcinoma: current methodologies[J]. Adv Anat Pathol, 2010, 9(4): 233-43. [12] Creager AJ, Geisinger KR. Int raoperative evaluation of sentinel lymph nodes for breast carcinoma: current methodologies[J]. Adv Anat Pathol, 2010, 9(4): 233-43. http://cn.bing.com/academic/profile?id=2028989906&encoded=0&v=paper_preview&mkt=zh-cn
[13] Ma HY, Progression on minimally invasive therapy of breast cancer[J]. Zhonghua Pu Wai Ji Chu Yu Lin Chuang Za Zhi, 2010, 17 (3): 214-8. [马宏岩. 乳腺癌微创治疗的研究进展[J]. 中华普 外基础与临床杂志, 2010, 17(3): 214-8.] [13] 马宏岩. 乳腺癌微创治疗的研究进展[J]. 中华普外基础与临床杂志, 2010, 17(3): 214-8. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201003003.htm Ma HY, Progression on minimally invasive therapy of breast cancer[J]. Zhonghua Pu Wai Ji Chu Yu Lin Chuang Za Zhi, 2010, 17(3): 214-8. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201003003.htm
[14] Wu SD, Fan Y, Xi W, et al. Single incision breast conservation surgery and cavity mirror the axillary lymph node resection in 2 cases[J]. Zhonghua Ru Xian Bing Za Zhi(Dian Zi Ban), 2010, 4(5): 62-3. [吴 硕东, 范莹, 希渥, 等. 单切口乳腺癌保留乳房手术并腔镜下腋窝 淋巴结切除术2例[J]. 中华乳腺病杂志(电子版), 2010, 4(5): 62-3.] [14] 吴硕东, 范莹, 希渥, 等. 单切口乳腺癌保留乳房手术并腔镜下腋窝淋巴结切除术2例[J]. 中华乳腺病杂志(电子版), 2010, 4(5): 62-3. http://www.cnki.com.cn/Article/CJFDTOTAL-ZHRD201005019.htm Wu SD, Fan Y, Xi W, et al. Single incision breast conservation surgery and cavity mirror the axillary lymph node resection in 2 cases[J]. Zhonghua Ru Xian Bing Za Zhi(Dian Zi Ban), 2010, 4(5): 62-3. http://www.cnki.com.cn/Article/CJFDTOTAL-ZHRD201005019.htm



 下载:
下载: